Hello all, this is my first post on here. Diagnosed hypothyroid March. I have a puzzling question that has not been answered by a thyroid facebook group that I follow. My Levo patient leaflet suggests that dosage changes can be implemented every 3/4 weeks but the NHS insist that changes must wait 6 weeks! As the NICE guidelines recommend treating until the symptoms disappear and another NICE document suggest changes every 4 weeks it seems that the NHS 6 week testing rule which generally only tests TSH is pointless and contradictory!!? Has anybody seen any research to this effect?? TIA
Levo increases: Hello all, this is my first post... - Thyroid UK
Levo increases
The reason for a six week gap is that is widely believed to be the time it takes for blood test levels to stabilise after a change of dose.
Much of the effect of a change, both on the person and on their blood test results, will occur sooner. But some changes continue for weeks, months, possibly years.
If we could have daily tests (TSH, FT4 and FT3), which is obviously fanciful, we might see the levels change significantly in the first few days, then slowly over the next weeks. We might even see some levels go up and then down (or down and then up) and move around a bit over a few weeks - albeit possibly only by small amounts. We would also be better placed to see that a dose change is needed and make it as soon as it is clear beyond doubt.
Discussing 3, 4 or 6 weeks is perfectly reasonable. But it does not help that some labs reject repeat tests within a short time (variable).
I do not believe that a GP should ignore the Patient Information Leaflet and NICE guidelines out of ignorance or unwillingness to test (or unwillingness of lab to process a test). They are right to make their own decision but it needs to be from understanding the clinical situation, etc. Diverging from PIL and NICE requires justification.
Thank you very much for your reply helvella. I am aware of the widely believed theory that levels can change over weeks/months but why would the drug companies and NICE state that changes can be made every 3/4 weeks if implementing this would be a problem and if Drs do not allow this. This means that severely ill people have to wait much much longer to achieve their optimal dose because there seems to be only the 6 week law!! Do you know of any research papers which examines these intervals?
Sorry hellvella I forgot to also query the need for 6 week testing if the patient is still extremely ill with hypo symptoms. Surely dose changes could be made earlier in accordance with NICE guidelines even if the labs will not test more often than 6 weekly?
Difficult.
If you do a thought experiment - imagine someone who is very ill with hypothyroidism. You decide to increase their dose every day and do so by 25 micrograms.
It is certain that the dose will shoot way past how much they need. Symptoms don't all resolve within a day, a week, a month, even a year or more.
At the same time, starting low and not raising soon enough is very poor practice. And yet we see it all too often.
The NICE guidelines appear to overcome that for many by using a formula-based replacement dose. But this too has problems. Many patients feel terrible if given that much all of a sudden. And many patients never need as much as the formula dictates.
My view is that at the very start of treatment, a lower should be used. Lower than the formula dictates. And adjusted according to factors like how long the person has been hypothyroid (as far as can be determined), how severe, etc.
Patient A, formula suggests 150 micrograms a day, and they are not old, do not have other diseases, etc. Maybe start on 50 and, if well-tolerated on Day 1, try 75 on Day 3, and 100 on Day 7. Then go for more spaced out increments.
Patient B, formula again suggests 150 micrograms a day but they have been very ill for a long time and have several other issues. Maybe start on 25, and wait a few days. Then increment by 25 and so on.
In both cases, if the person feels they are running out by end of day, that would be a key indication that more is needed.
I'd also suggest split dosing - even down to 12.5 micrograms or less in each dose.
This is all a matter of how it appears to me - not based on research, science, or anything else.
Remembering two prime issues.
Ramping up dose too fast can overwhelm the body.
Not providing as much as the body needs across 24 hours a day results in a roller coaster between have some, albeit still inadequate, levothyroxine, and using it up and having none.
Both are bad.
(In hospitalised cases, treatment of myxoedema coma is usually high doses of levothyroxine, sometimes injected, and possibly also liothyronine. But that is an emergency.)
None of the above does anything towards recognising those who need liothyronine and will end up putting such patients through the "traditional" process of assuming levothyroxine only until (eventually) proved otherwise. However, it might well be better to use liothyronine very early on. That is another story altogether.
As vast majority of GP’s only look at TSH we need TSH as high as possible before retesting
In practice many patients find that means waiting 6-10 weeks
Always test as early as possible in morning before eating or drinking anything other than water and last dose levothyroxine 24 hours before test
Very common to need to start on low dose levothyroxine and increase SLOWLY upwards, especially if been hypothyroid a long time before diagnosis
How much levothyroxine are you currently taking
What were your thyroid and vitamin levels at diagnosis
guidelines on dose levothyroxine by weight
Even if we frequently don’t start on full replacement dose, most people need to increase levothyroxine dose slowly upwards in 25mcg steps (retesting 6-8 weeks after each increase) until eventually on, or near full replacement dose
NICE guidelines on full replacement dose
nice.org.uk/guidance/ng145/...
1.3.6
Consider starting levothyroxine at a dosage of 1.6 micrograms per kilogram of body weight per day (rounded to the nearest 25 micrograms) for adults under 65 with primary hypothyroidism and no history of cardiovascular disease.
Also here
cks.nice.org.uk/topics/hypo...
gp-update.co.uk/Latest-Upda...
Traditionally we have tended to start patients on a low dose of levothyroxine and titrate it up over a period of months. RCT evidence suggests that for the majority of patients this is not necessary and may waste resources.
For patients aged >60y or with ischaemic heart disease, start levothyroxine at 25–50μg daily and titrate up every 3 to 6 weeks as tolerated.
For ALL other patients start at full replacement dose. For most this will equate to 1.6 μg/kg/day (approximately 100μg for a 60kg woman and 125μg for a 75kg man).
If you are starting treatment for subclinical hypothyroidism, this article advises starting at a dose close to the full treatment dose on the basis that it is difficult to assess symptom response unless a therapeutic dose has been trialled.
BMJ also clear on dose required
bestpractice.bmj.com/topics...
Guidelines are just that ....guidelines. Some people need more some less
healthunlocked.com/thyroidu...
Many thanks for the links Slow Dragon. I have still been unable to find research papers on the 6 week testing/ dose change recommendation though!
ncbi.nlm.nih.gov/pmc/articl...
Monitoring thyroid function during levothyroxine replacement
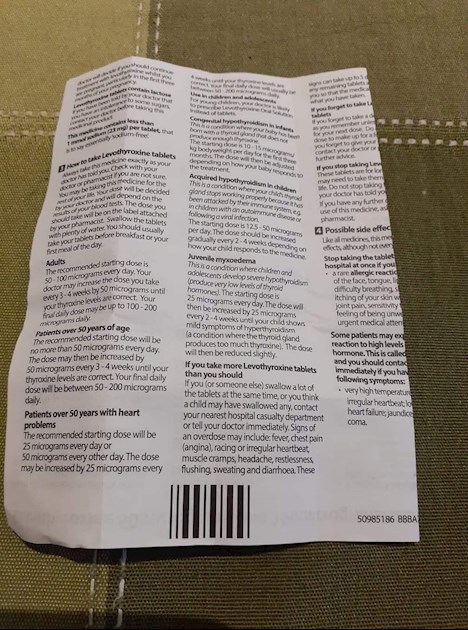
When initiating levothyroxine therapy, serum TSH should be measured to monitor for adequate replacement. TSH can take up to 4 months to normalize, even when starting on a full dose replacement regimen, due to thyrotroph hyperplasia. It is recommended that the TSH is measured 6–8 weeks after initiation of, or a change in levothyroxine dose.
I certainly find, from practice experience, that it’s best to wait 8-10 weeks before testing after any dose change in levothyroxine