hi, i was recently put on 25mcg Levothyroxine and 5mg of folic acid and 10mg Propranolol but my symptoms have not changed at all but GP said all bloods are now ok. i had private bloods done, can anyone suggest anything that will help me please, i’m attaching my private bloods
hi, i’m a newbie with crazy symptoms, can anyon... - Thyroid UK
hi, i’m a newbie with crazy symptoms, can anyone understand these blood results please
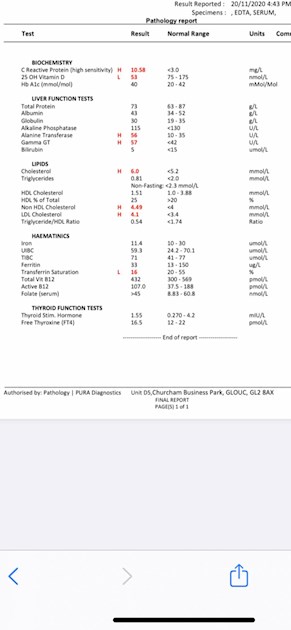
Do you have a value for your free T3? Your iron is low, you should start supplementing asap. I recommend ferrous fumarate rather than ferrous sulphate as it's easier on the stomach. Your C-reactive protein is high which indicates inflammation in your body. Do you follow a gluten/dairy free diet?
2020diagnosed
How recently did you start Levo?
Normal starting dose is 50mcg unless a child, elderly or have a heart condition.
Retest should be done 6 weeks after starting, increase dose by 25mcg, retest 6-8 weeks later, repeat until your levels are where they need to be for you to feel well.
The aim of a treated Hypo patient on Levo, generally, is for TSH to be 1 or lower with FT4 and FT3 in the upper part of their reference ranges if that is where you feel well.
Your TSH is 1.55 (0.27-4.2) and FT4 is 16.5 (12-22). Your FT4 is only 45% through range so these results suggest an increase in your dose of Levo. Wait 6-8 weeks then retest and make sure you test TSH, FT4 and FT3 all together. FT3 is the most important test as this tells you whether you are converting T4 to T3 well enough, and whether you are overmedicated.
The cheapest way to get just TSH, FT4 and FT3 tested is with Monitor My Health which is an NHS lab who offer a fingerprick test to the general public for £29, discounted with the code in this link:
thyroiduk.org/getting-a-dia...
If you also require antibodies testing then use Blue Horizon or Medichecks.
**
Why have you been prescribed Propranolol?
**
Have you had thyroid antibodies tested confirming autoimmune thyroid disease aka Hasimoto's?
**
Your results are very difficult to read (too small) even on my large PC monitor. It would help if you could edit your opening post, remove the picture and resubmit the picture zooming in on the results only, leave out all that unnecessary blank space.
From what I can make out:
Your C-Reactive Protein result is high, this is an inflammation marker.
**
Your Vit D is marked as Low, I think it may be 53nmol/L, if so then you should consider supplementing to improve this to the level recommended by the Vit D Council/Vit D Society which is 100-150nmol/L. Supplementing with 4,000-5,000iu D3 daily would be suggested by the Vit D Council. Retest after 3 months.
When you have reached the recommended level then you'll need a maintenance dose to keep it there, which may be 2000iu daily, maybe more or less, maybe less in summer than winter, it's trial and error so it's recommended to retest once or twice a year to keep within the recommended range. You can do this with a private fingerprick blood spot test with an NHS lab which offers this test to the general public:
Doctors don't know, because they're not taught much about nutrients, but there are important cofactors needed when taking D3 as recommended by the Vit D Council.
D3 aids absorption of calcium from food and Vit K2-MK7 directs the calcium to bones and teeth where it is needed and away from arteries and soft tissues where it can be deposited and cause problems such as hardening of the arteries, kidney stones, etc.
D3 and K2 are fat soluble so should be taken with the fattiest meal of the day, D3 four hours away from thyroid meds if taking D3 as tablets/capsules/softgels, no necessity if using an oral spray.
Magnesium helps D3 to work. We need Magnesium so that the body utilises D3, it's required to convert Vit D into it's active form. So it's important we ensure we take magnesium when supplementing with D3.
Magnesium comes in different forms, check to see which would suit you best and as it's calming it's best taken in the evening, four hours away from thyroid meds if taking magnesium as tablets/capsules, no necessity if using topical forms of magnesium.
naturalnews.com/046401_magn...
drjockers.com/best-magnesiu...
**
High Cholesterol is a symptom of underactive thyroid and may resolve itself when optimally medicated with Levo.
**
Optimal levels for an iron panel according to rt3-adrenals.org/Iron_test_... are:
Serum iron: 55 to 70% of the range, higher end for men. If the range for your test is 10-30 (it's not clear) then yours is 7% through range which is very low.
Saturation: optimal is 35 to 45%, higher end for men - yours is 16% so very low.
Total Iron Binding Capacity: Low in range indicates lack of capacity for additional iron, High in range indicates body's need for supplemental iron - yours is high in range.
Ferritin: Low level virtually always indicates need for iron supplementation - I think your result is 33 which is low.
You should discuss your iron panel with your GP, it looks very much like you should be prescribed iron tablets. Ask for a full blood count to see if you are anaemic.
**
Active B12 (the more important test) is over 100 so that is good. Do you supplement?
**
Folate is greater than 45 which suggests that you no longer need the 5mg folic acid, that's usually a temporary thing until folate level is optimal then it just needs maintaining with possibly a low dose of methylfolate (400mcg) which you would find in a good quality B Complex. This will also maintain your B12 level and keep all B vitamins balanced. Consider Thorne Basic B or Igennus Super B.
**
Don't start all supplements at once. Start with one, give it a week or two and if no adverse reaction then add the next one. Again, wait a week or two and if no adverse reaction add the next one. Continue like this. If you do have any adverse reaction then you will know what caused it.
oh wow you’re a mind of information thank you so much. i used an online test so i don’t know why they didn’t test my free T3. i’ve been on 25mcg for 8 weeks now and GP just says you’re dose is fine as bloods are ok now. i will work on all of your suggestions. thank you again for your time
2020diagnosedFT3 wasn't tested because that bundle you chose doesn't include the full thyroid panel. You might have been better with just the thyroid/vitamin panel - if that is a Blue Horizon test that would be the Thyroid Premium Gold.
If you are going to self supplement with iron then it's essential to monitor your levels regularly, say every 3 months. However, I would recommend that you discuss the iron results with your GP and ask for the full blood count as well to see if you are anaemic. Let your GP prescribe and do the regular monitoring.
If you still have hypothyroid symptoms then your GP should increase your dose. I'm on my tablet and don't have links, but SlowDragon may pop along and put the information about titrating dose.
For full Thyroid evaluation you need TSH, FT4 and FT3 plus both TPO and TG thyroid antibodies tested. Also EXTREMELY important to test vitamin D, folate, ferritin and B12
Low vitamin levels are extremely common, especially if you have autoimmune thyroid disease (Hashimoto's) diagnosed by raised Thyroid antibodies
Ask GP to test thyroid antibodies, or test privately
Recommended on here that all thyroid blood tests should ideally be done as early as possible in morning and before eating or drinking anything other than water .
Last dose of Levothyroxine 24 hours prior to blood test. (taking delayed dose immediately after blood draw).
This gives highest TSH, lowest FT4 and most consistent results. (Patient to patient tip)
Private tests are available as NHS currently rarely tests Ft3 or thyroid antibodies or all relevant vitamins
List of private testing options
thyroiduk.org/getting-a-dia...
Medichecks Thyroid plus antibodies and vitamins
medichecks.com/products/adv...
Thriva Thyroid plus antibodies and vitamins By DIY fingerpick test
Thriva also offer just vitamin testing
Blue Horizon Thyroid Premium Gold includes antibodies, cortisol and vitamins by DIY fingerprick test
bluehorizonbloodtests.co.uk...
If you can get GP to test vitamins and antibodies then cheapest option for just TSH, FT4 and FT3
£29 (via NHS private service ) and 10% off down to £26.10 if go on thyroid uk for code
thyroiduk.org/getting-a-dia...
monitormyhealth.org.uk/thyr...
Request GP do full iron panel test for anaemia
Ferritin is low, saturation is below range
Vitamin D is too low.
thank you i will request this from my GP although they are very unhelpful, thanks for your advice
Yes, that’s an almost universal experience....hence over 112,000 members on here
If you can’t get full iron panel test for anaemia via GP, you can order one via Medichecks
humanbean or SeasideSusie can help you decipher the results
Vitamin D GP will often only prescribe to bring levels to 50nmol.Some areas will prescribe to bring levels to 75nmol
leedsformulary.nhs.uk/docs/...
GP should advise on self supplementing if over 50nmol, but under 75nmol (but they rarely do)
mm.wirral.nhs.uk/document_u...
NHS Guidelines on dose vitamin D required
ouh.nhs.uk/osteoporosis/use...
But with Hashimoto’s, improving to around 80nmol or 100nmol by self supplementing may be better
ncbi.nlm.nih.gov/pubmed/218...
vitamindsociety.org/pdf/Vit...
Once you Improve level, very likely you will need on going maintenance dose to keep it there.
Test twice yearly via vitamindtest.org.uk
Vitamin D mouth spray by Better You is very effective as it avoids poor gut function. There’s a version made that also contains vitamin K2 Mk7
It’s trial and error what dose we need, with hashimoto’s we frequently need higher dose than average
Calculator for working out dose you may need to bring level to 40ng/ml = 100nmol
grassrootshealth.net/projec...
Government recommends everyone supplement October to April
gov.uk/government/news/phe-...
Taking too much vitamin D is not a good idea
chriskresser.com/vitamin-d-...
With your Vit D, are you also taking it's important cofactors - magnesium and Vit K2-MK7?
Magnesium best taken in the afternoon or evening, but must be four hours away from levothyroxine
betterbones.com/bone-nutrit...
medicalnewstoday.com/articl...
livescience.com/61866-magne...
sciencedaily.com/releases/2...
Vitamin K2 mk7
Propranolol will reduce your T4 to T3 conversion and this may be affecting you. If you need a beta blocker they should use a different one. Propranolol is used to treat HYPERthyroidism.
oh that’s interesting, thank you
Why was propranolol prescribed?
Headache? Palpitations? Anxiety?
All are hypothyroid symptoms
As jimh111 says propranolol will affect how levothyroxine works and is best avoided
pubmed.ncbi.nlm.nih.gov/168...
Propranolol also lowers parathyroid hormones and if vitamin D deficient that’s not good
labtestsonline.org.uk/tests...
See - is there anything else I should know
Drugs that may decrease PTH include cimetidine and propranolol.
Standard starter dose of levothyroxine is 50mcg
Bloods should be retested 6-8 weeks after each dose increase
guidelines on dose levothyroxine by weight
Even if we frequently don’t start on full replacement dose, most people need to increase levothyroxine dose slowly upwards in 25mcg steps (retesting 6-8 weeks after each increase) until on, or near, full replacement dose
NICE guidelines on full replacement dose
nice.org.uk/guidance/ng145/...
1.3.6
Consider starting levothyroxine at a dosage of 1.6 micrograms per kilogram of body weight per day (rounded to the nearest 25 micrograms) for adults under 65 with primary hypothyroidism and no history of cardiovascular disease.
Also here
cks.nice.org.uk/topics/hypo...
gp-update.co.uk/Latest-Upda...
Traditionally we have tended to start patients on a low dose of levothyroxine and titrate it up over a period of months.
RCT evidence suggests that for the majority of patients this is not necessary and may waste resources.
For patients aged >60y or with ischaemic heart disease, start levothyroxine at 25–50μg daily and titrate up every 3 to 6 weeks as tolerated.
For ALL other patients start at full replacement dose. For most this will equate to 1.6 μg/kg/day (approximately 100μg for a 60kg woman and 125μg for a 75kg man).
If you are starting treatment for subclinical hypothyroidism, this article advises starting at a dose close to the full treatment dose on the basis that it is difficult to assess symptom response unless a therapeutic dose has been trialled.
A small Dutch double-blind cross-over study (ArchIntMed 2010;170:1996) demonstrated that night time rather than morning dosing improved TSH suppression and free T4 measurements, but made no difference to subjective wellbeing. It is reasonable to take levothyroxine at night rather than in the morning, especially for individuals who do not eat late at night.
BMJ also clear on dose required
Thank you for your reply. i should have added that i have Rheumatoid Arthritis and take 100mg Azathioprine. I was prescribed the Propranolol for palpitations and anxiety. i have just had a call from the GP saying my Thyroid scan has shown up a cyst nodule (i think that’s what she said) and that i need the scan repeated in 6 months. Also i’m having a 24hr ECG fitted today as on my last doctors visit she heard an extra heartbeat when listening to my chest. i have such crazy symptoms, i will list as many as i can - slow brain function, absent feeling in my brain, burning feet/hands and face, pins and needles and numbness in hands and lower arms, memory loss, brain fog, headaches, dizziness, nausea, anxiety, no appetite, chronic fatigue. i did have abdominal pains for over a year but since i’ve been on Levothyroxine the abdominal pain has stopped, low temperatures, freezing cold. All of this has been blamed on depression for years but i actually don’t feel depressed i just feel so ill. I’ve tried so many different antidepressants that have never helped at all. Sorry if this sounds like a ramble, i just feel like i’m going crazy. thank you.
So you have RA and your on a immunosuppressive drug... This could be the reason behind your palpitations and anxiety and recent nodule on thyroid!
I was on Stelara for a year 2015 to 2016 when my MULTIPLE thyroid checks revealed a couple of nodules during that year. I would complain about severe panic attacks and racing pulse , wore a heart monitor for a couple of days no issues recorded and as soon as I would do my monthly injections I could taste the Stelar injection in my throat (strange taste, chemical) and panic attacks and anxiety for couple of days after the injections and the doctors kept saying not possible..... October 2016 again horrible racing pulse and panic attacks (random) but this seemed to be only around my injections my eye popped out of its socket (you couldn’t see the color of my eye) and it bulged out (hurt) they did another FNB and this one came back as thyroid cancer.
Had thyroidectomy and stopped Stelara and developed severe psoriatic arthritis that I did not have prior to surgery... Been on Cosentyx (2yrs) now and for 2 days after these injection I get palpitations and anxiety the same way I did with Stelara, coincidence maybe.
Im not saying this is your issue but its possible.
it’s a mind field once you start looking into stuff, i am just so overwhelmed by to much information that i can’t make any sense of it all and the random symptoms that i tell my doctor and RH about and they just ignore it. i’ve really started to push them to try to get answers and my GP actually laughed at me so i had bloods done privately 3 month’s ago and again recently. i have to say that by doing this they have been a bit more helpful but not active enough to to put everything together and work out what on earth is going on. i feel pushed from pillar to post but not getting any actual answers and i getting desperate now. you have been through a lot too and it’s not on. i have RH ringing me on the 5th December do i will ask him if the medication could be causing any of my symptoms, thank you and wishing you good health
Hi,I'm quite new to this site too and I came here for exactly the reasons you have. Unfortunately I still have no diagnosis and I also had my GP laugh at me when I was telling her all my symptoms. I decided there and then not to go back. How dare they laugh at their patients. I had private blood tests done that came back with several problems and yet they still tell me I'm normal. I'm speaking to someone tomorrow to ask them for a referral to a private endo. I already know its not going to be easy but I will not be fobbed off. This site has been a life saver for me. Good luck with your journey.