Hi all.
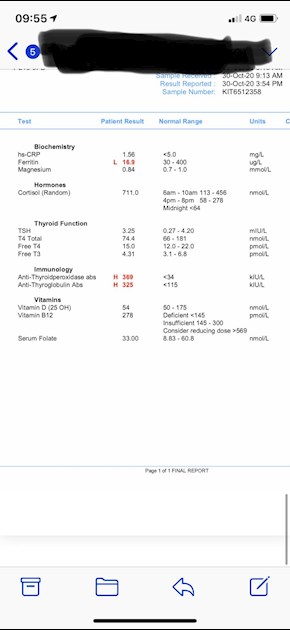
As recommended I did some bloods. I am posting the results and would be so grateful for any advice. The breathlessness is hacking me off now!! As are numerous other symptoms. 🙄
Thanks I’m advance!!
Hi all.
As recommended I did some bloods. I am posting the results and would be so grateful for any advice. The breathlessness is hacking me off now!! As are numerous other symptoms. 🙄
Thanks I’m advance!!
See GP
Ferritin is extremely low. You need full iron panel test for anaemia
Likely to need iron infusion, if not that, almost certainly ferrous fumerate supplements
Never supplement iron without doing full iron panel test for anaemia first
Eating iron rich foods like liver or liver pate once a week plus other red meat, pumpkin seeds and dark chocolate, plus daily orange juice or other vitamin C rich drink can help improve iron absorption
List of iron rich foods
Links about iron and ferritin
irondisorders.org/Websites/...
drhedberg.com/ferritin-hypo...
This is interesting because I have noticed that many patients with Hashimoto’s disease and hypothyroidism, start to feel worse when their ferritin drops below 80 and usually there is hair loss when it drops below 50.
Breathlessness is common symptom of anaemia
B12 and folate are too low. But GP unlikely to agree
Ideally GP should run further testing for Pernicious Anaemia before starting any B vitamins. But they likely won’t
You probably will need to self supplement
supplement a good quality daily vitamin B complex, one with folate in (not folic acid) may be beneficial.
This can help keep all B vitamins in balance and will help improve B12 levels too
Difference between folate and folic acid
chriskresser.com/folate-vs-...
Many Hashimoto’s patients have MTHFR gene variation and can have trouble processing folic acid.
thyroidpharmacist.com/artic...
B vitamins best taken after breakfast
Igennus Super B is good quality and cheap vitamin B complex. Contains folate. Full dose is two tablets per day. Many/most people may only need one tablet per day. Certainly only start on one per day (or even half tablet per day for first couple of weeks)
Or Thorne Basic B is another option that contains folate, but large capsules
If you are taking vitamin B complex, or any supplements containing biotin, remember to stop these 7 days before ALL blood tests, as biotin can falsely affect test results
endo.confex.com/endo/2016en...
endocrinenews.endocrine.org...
Low B12 symptoms
b12deficiency.info/signs-an...
With such low B12 result taking a B12 supplement as well as a B Complex (to balance all the B vitamins) initially for first 2-4 months, then once your serum B12 is over 500 (or Active B12 level has reached 70), stop the B12 and just carry on with the B Complex.
B12 sublingual lozenges
amazon.co.uk/Jarrow-Methylc...
cytoplan.co.uk/vitamins/vit...
All your vitamins are terrible, because you are extremely under medicated
Vitamin D is too low, but probably not low enough for GP to prescribe
GP will often only prescribe to bring levels to 50nmol.
Some areas will prescribe to bring levels to 75nmol
leedsformulary.nhs.uk/docs/...
GP should advise on self supplementing if over 50nmol, but under 75nmol (but they rarely do)
mm.wirral.nhs.uk/document_u...
NHS Guidelines on dose vitamin D required
ouh.nhs.uk/osteoporosis/use...
But with Hashimoto’s, improving to around 80nmol or 100nmol by self supplementing may be better
ncbi.nlm.nih.gov/pubmed/218...
vitamindsociety.org/pdf/Vit...
Once you Improve level, very likely you will need on going maintenance dose to keep it there.
Test twice yearly via vitamindtest.org.uk
Vitamin D mouth spray by Better You is very effective as it avoids poor gut function. There’s a version made that also contains vitamin K2 Mk7
It’s trial and error what dose we need, with hashimoto’s we frequently need higher dose than average
Calculator for working out dose you may need to bring level to 40ng/ml = 100nmol
grassrootshealth.net/projec...
Government recommends everyone supplement October to April
gov.uk/government/news/phe-...
With your Vit D, are you also taking it's important cofactors - magnesium and Vit K2-MK7?
Magnesium best taken in the afternoon or evening, but must be four hours away from levothyroxine
betterbones.com/bone-nutrit...
medicalnewstoday.com/articl...
livescience.com/61866-magne...
sciencedaily.com/releases/2...
Vitamin K2 mk7
Vitamin levels are all so low because you are under medicated and on too low a dose of levothyroxine
Request dose 25mcg increase in dose to 100mcg daily
Suggest you increase slowly, initially to 75mcg/100mcg alternate days and then to 100mcg daily
Are you currently taking Teva brand? This upsets many people
While vitamins are so low it’s likely best to increase levo slowly
Working on improving low vitamins at same time
Only add one supplement at a time and wait 2 weeks to assess any changes
Perhaps Vitamin D first, then add vitamin B complex, then magnesium, then B12
No other medication or supplements at same as Levothyroxine, leave at least 2 hour gap.
Some like iron, calcium, magnesium, HRT, omeprazole or vitamin D should be four hours away
(Time gap doesn't apply to Vitamin D mouth spray)
Many people find Levothyroxine brands are not interchangeable.
Once you find a brand that suits you, best to make sure to only get that one at each prescription.
Watch out for brand change when dose is increased or at repeat prescription.
Many patients do NOT get on well with Teva brand of Levothyroxine. Teva contains mannitol as a filler, which seems to be possible cause of problems. Teva is the only brand that makes 75mcg tablet. So if avoiding Teva for 75mcg dose ask for 25mcg to add to 50mcg or just extra 50mcg tablets to cut in half
Are you currently taking Teva?
Teva, Aristo and Glenmark are the only lactose free tablets
healthunlocked.com/thyroidu...
Teva poll
healthunlocked.com/thyroidu...
academic.oup.com/jcem/artic...
Physicians should: 1) alert patients that preparations may be switched at the pharmacy; 2) encourage patients to ask to remain on the same preparation at every pharmacy refill; and 3) make sure patients understand the need to have their TSH retested and the potential for dosing readjusted every time their LT4 preparation is switched (18).
Levothyroxine is an extremely fussy hormone and should always be taken on an empty stomach and then nothing apart from water for at least an hour after
Many people take Levothyroxine soon after waking, but it may be more convenient and perhaps more effective taken at bedtime
verywellhealth.com/best-tim...
If you normally take levothyroxine at bedtime/in night ...adjust timings as follows prior to blood test
If testing Monday morning, delay Saturday evening dose levothyroxine until Sunday morning. Delay Sunday evening dose levothyroxine until after blood test on Monday morning. Take Monday evening dose levothyroxine as per normal
guidelines on dose levothyroxine by weight
Even if we don’t start on full replacement dose, most people need to increase levothyroxine dose slowly upwards in 25mcg steps (retesting 6-8 weeks after each increase) until on full replacement dose
NICE guidelines on full replacement dose
nice.org.uk/guidance/ng145/...
1.3.6
Consider starting levothyroxine at a dosage of 1.6 micrograms per kilogram of body weight per day (rounded to the nearest 25 micrograms) for adults under 65 with primary hypothyroidism and no history of cardiovascular disease.
gp-update.co.uk/Latest-Upda...
Traditionally we have tended to start patients on a low dose of levothyroxine and titrate it up over a period of months.
RCT evidence suggests that for the majority of patients this is not necessary and may waste resources.
For patients aged >60y or with ischaemic heart disease, start levothyroxine at 25–50μg daily and titrate up every 3 to 6 weeks as tolerated.
For ALL other patients start at full replacement dose. For most this will equate to 1.6 μg/kg/day (approximately 100μg for a 60kg woman and 125μg for a 75kg man).
If you are starting treatment for subclinical hypothyroidism, this article advises starting at a dose close to the full treatment dose on the basis that it is difficult to assess symptom response unless a therapeutic dose has been trialled.
A small Dutch double-blind cross-over study (ArchIntMed 2010;170:1996) demonstrated that night time rather than morning dosing improved TSH suppression and free T4 measurements, but made no difference to subjective wellbeing. It is reasonable to take levothyroxine at night rather than in the morning, especially for individuals who do not eat late at night.
BMJ also clear on dose required
bestpractice.bmj.com/topics...
Getting levothyroxine dose slowly increased up in 25mcg steps (bloods tested 6-8 weeks after each dose increase) and at same time also working on improving low vitamin levels will significantly improve symptoms
Last point
Something to consider after getting vitamins optimal and levothyroxine fine tuned
you have high antibodies this is Hashimoto's, (also known by medics here in UK more commonly as autoimmune thyroid disease).
Hashimoto's frequently affects the gut and leads to low stomach acid and then low vitamin levels
Low vitamin levels affect Thyroid hormone working, as you can see
Poor gut function can lead leaky gut (literally holes in gut wall) this can cause food intolerances. Most common by far is gluten. Dairy is second most common.
According to Izabella Wentz the Thyroid Pharmacist approx 5% with Hashimoto's are coeliac, but over 80% find gluten free diet helps, sometimes significantly. Either due to direct gluten intolerance (no test available) or due to leaky gut and gluten causing molecular mimicry (see Amy Myers link)
Changing to a strictly gluten free diet may help reduce symptoms, help gut heal and slowly lower TPO antibodies
While still eating high gluten diet ask GP for coeliac blood test first or buy test online for under £20, just to rule it out first
healthcheckshop.co.uk/store...?
Assuming test is negative you can immediately go on strictly gluten free diet
(If test is positive you will need to remain on high gluten diet until endoscopy, maximum 6 weeks wait officially)
Trying gluten free diet for 3-6 months. If no noticeable improvement then reintroduce gluten and see if symptoms get worse
chriskresser.com/the-gluten...
amymyersmd.com/2018/04/3-re...
thyroidpharmacist.com/artic...
drknews.com/changing-your-d...
restartmed.com/hashimotos-g...
Non Coeliac Gluten sensitivity (NCGS) and autoimmune disease
ncbi.nlm.nih.gov/pubmed/296...
The predominance of Hashimoto thyroiditis represents an interesting finding, since it has been indirectly confirmed by an Italian study, showing that autoimmune thyroid disease is a risk factor for the evolution towards NCGS in a group of patients with minimal duodenal inflammation. On these bases, an autoimmune stigma in NCGS is strongly supported
ncbi.nlm.nih.gov/pubmed/300...
The obtained results suggest that the gluten-free diet may bring clinical benefits to women with autoimmune thyroid disease
nuclmed.gr/wp/wp-content/up...
In summary, whereas it is not yet clear whether a gluten free diet can prevent autoimmune diseases, it is worth mentioning that HT patients with or without CD benefit from a diet low in gluten as far as the progression and the potential disease complications are concerned
restartmed.com/hashimotos-g...
Despite the fact that 5-10% of patients have Celiac disease, in my experience and in the experience of many other physicians, at least 80% + of patients with Hashimoto's who go gluten-free notice a reduction in their symptoms almost immediately.
Thanks Slowdragon. Currently at work and so will have a good read of your points when I finish. Which I am so eager to do now!!!
Thanks so much.
Important to address low iron and ferritin ASAP
Don’t get fobbed off by GP
Thanks for the info and links. I have emailed gp and endo but we’ll see.
I don’t suppose anyone knows how reliable the cortisol blood tests are? And if my levels although raised are consider problematic? I am not on steroids and don’t do stress either lol.
High cortisol is common when under medicated and hypothyroid as adrenals try to compensate for lack of thyroid hormones
I was literally just reading that. Thank so much. You super!! Hopefully I’ll get some sort of response from gp or endo this week. If they’re not too busy with covid that is.
Thanks again.
So... I had a call with doctor. Didn’t want to go from bloods by blue horizon so have to have more which I have booked for Tuesday. Fortunately I had emailed the endo department and he actually received it and asked my gp to up my dose. Result!! The surgery text me letting me know. Still doing more bloods but tsh only to be tested in 3 months.
Thank you so much everyone. Without your advice I would still be without a light at the end of a tunnel. So I am very grateful.
Incidentally all this reading has made me wonder about the genetic link. My dad has always suffered like me. He was diagnosed with M.E in 1987 and is much improved but suffers with aches and fatigue. I asked him to have some bloods a couple of years ago and he has found the results for me. He isn’t on any meds and to my uneducated eye they don’t seem too bad but I wonder if I could ask you knowledgeable lot to glance over them and tell me if you agree?
Tsh 1.42 range 0.270 - 4.200
Free t 16.81 range 12 - 22
Total t4 109.3 range 59 - 154
Free t3 4.5 range 3.1 - 6.8
Tgab. 123. Range 0 - 115
TPOab. 10.12. range 0 - 34
I’m guessing I was clutching at straws 🙄
Yes. Definitely. Thank you. You said what I was thinking so maybe I am learning!!
@survivalmode obviously these are replies to my issues but there are a lot of links and info crammed in. Hopefully some far more educated about all this will assist but in the meantime you can see where you may need to start.