ranges from medichecks.
thyroid results: ranges from medichecks. - Thyroid UK
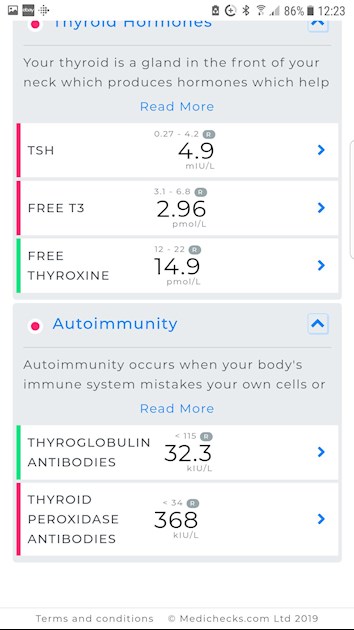
thyroid results
Original post
healthunlocked.com/thyroidu...
Other results:
giggy63
after these results have ad my levothyroxine increased from 75 to 100, but still feel tired and aching most of the time
So an increase, based on your thyroid results, was the right thing to do. You should be retested 6-8 weeks after the increase, if necessary a further increase of 25mcg, retest 6-8 weeks later, repeat until your levels are where they need to be for you to feel well. The aim of a treated Hypo patient on Levo, generally, is for TSH to be 1 or below with FT4 and FT3 in the upper part of their reference ranges if that is where you feel well.
**
When doing thyroid tests, we advise:
* Book the first appointment of the morning, or with private tests at home no later than 9am. This is because TSH is highest early morning and lowers throughout the day. If we are looking for a diagnosis of hypothyroidism, or looking for an increase in dose or to avoid a reduction then we need TSH to be as high as possible.
* Fast overnight - have your evening meal/supper as normal the night before but delay breakfast on the day of the test and drink water only until after the blood draw. Eating may lower TSH, coffee affects TSH so it's possible that other caffeine containing drinks may also affect TSH.
* When taking thyroid hormone replacement, last dose of Levo should be 24 hours before blood draw, if taking NDT or T3 then last dose should be 8-12 hours before blood draw. Adjust timing the day before if necessary. This avoids measuring hormone levels at their peak after ingestion of hormone replacement. Take your thyroid meds after the blood draw. Taking your dose too close to the blood draw will give false high results, leaving any longer gap will give false low results.
* If you take Biotin or a B Complex containing Biotin (B7), leave this off for 7 days before any blood test. This is because if Biotin is used in the testing procedure it can give false results (most labs use Biotin in the assay).
These are patient to patient tips which we don't discuss with doctors or phlebotomists.
**
Also, do you take your Levo on an empty stomach, one hour before or two hours after food, with a glass of water only, no tea, coffee, milk, etc, and water only for an hour either side (as absorption will be affected otherwise). Take any other medication and supplements 2 hours away from Levo, some need 4 hours.
**
Your raised thyroid peroxidase antibodies suggest that you are positive for autoimmune thyroid disease aka Hashimoto's which is where the thyroid is attacked and gradually destroyed. Did you know this?
Fluctuations in symptoms and test results are common with Hashi's.
Most doctors dismiss antibodies as being of no importance and know little or nothing about Hashi's and how it affects the patient, test results and symptoms. You need to read, learn, understand and help yourself where Hashi's is concerned.
Some members have found that adopting a strict gluten free diet can help, although there is no guarantee.
Gluten contains gliadin (a protein) which is thought to trigger autoimmune attacks so eliminating gluten can help reduce these attacks.
You don't need to be gluten sensitive or have Coeliac disease for a gluten free diet to help.
Gluten/thyroid connection: chriskresser.com/the-gluten...
stopthethyroidmadness.com/h...
stopthethyroidmadness.com/h...
hypothyroidmom.com/hashimot...
thyroiduk.org.uk/tuk/about_...
Supplementing with selenium l-selenomethionine 200mcg daily is said to help reduce the antibodies, as can keeping TSH suppressed.
**
From your other posts:
Folate: 3.68 - this is below range.This puts you in the "indeterminate" zone (rather than "deficiency" zone according to cks.nice.org.uk/anaemia-b12... which says
Folate level
◦Serum folate of less than 7 nanomol/L (3 micrograms/L) is used as a guide to indicate folate deficiency.
◦However, there is an indeterminate zone with folate levels of 7–10 nanomol/L (3–4.5 micrograms/L), so low folate should be interpreted as suggestive of deficiency and not diagnostic.
You should discuss this with your GP in the light of the comments above from NICE Clinical Knowledge Summary which your GP will have access to.
**
Active B12: 90.5 - this is OK. Below 70 suggests testing for B12 deficiency so you are well over that level. I like mine to be over 100.
**
Vit D: 66.7nmol/L - The Vit D Council recommends a level of 125nmol/L and the Vit D Society recommends a level of 100-150nmol/L.
To reach the recommended level from your current level, based on the Vit D Council's suggestions you could supplement with around 3,500iu D3 daily
Retest after 3 months.
Once you have reached the recommended level then you'll need a maintenance dose to keep it there, which may be 2000iu daily, maybe more or less, maybe less in summer than winter, it's trial and error so it's recommended to retest once or twice a year to keep within the recommended range. You can do this with a private fingerprick blood spot test with an NHS lab which offers this test to the general public:
Doctors don't know, because they're not taught much about nutrients, but there are important cofactors needed when taking D3 as recommended by the Vit D Council.
D3 aids absorption of calcium from food and Vit K2-MK7 directs the calcium to bones and teeth where it is needed and away from arteries and soft tissues where it can be deposited and cause problems such as hardening of the arteries, kidney stones, etc.
D3 and K2 are fat soluble so should be taken with the fattiest meal of the day, D3 four hours away from thyroid meds if taking D3 as tablets/capsules/softgels, no necessity if using an oral spray.
Magnesium helps D3 to work. We need Magnesium so that the body utilises D3, it's required to convert Vit D into it's active form. So it's important we ensure we take magnesium when supplementing with D3.
Magnesium comes in different forms, check to see which would suit you best and as it's calming it's best taken in the evening, four hours away from thyroid meds if taking magnesium as tablets/capsules, no necessity if using topical forms of magnesium.
naturalnews.com/046401_magn...
drjockers.com/best-magnesiu...
**
Ferritin: 58.6 (13-150) - this is low. Ferritin is recommended to be half way through range. Don't consider taking an iron supplement unless you do an iron panel to see if you have iron deficiency and a full blood count to see if you have anaemia. If you already have a decent level of serum iron and a good saturation percentage then taking iron tablets can push your iron level even higher, too much iron is as bad as too little.
You can help raise your level by eating liver regularly, maximum 200g per week due to it's high Vit A content, also liver pate, black pudding, and including lots of iron rich foods in your diet
apjcn.nhri.org.tw/server/in...
**
We need optimal nutrient levels for thyroid hormone to work properly, and low nutrient levels can bring their own symptoms as well.
**
Don't start all supplements at once. Start with one, give it a week or two and if no adverse reaction then add the next one. Again, wait a week or two and if no adverse reaction add the next one. Continue like this. If you do have any adverse reaction then you will know what caused it.
**
CRP is a little over range. This is a non-specific inflammation marker and Hashi's can cause inflammation.
You have high antibodies this confirms cause of your hypothyroidism is Hashimoto's, (also known by medics here in UK more commonly as autoimmune thyroid disease).
Hashimoto's frequently affects the gut and leads to low stomach acid and then low vitamin levels
Low vitamin levels affect Thyroid hormone working
Poor gut function can lead leaky gut (literally holes in gut wall) this can cause food intolerances. Most common by far is gluten. Dairy is second most common.
According to Izabella Wentz the Thyroid Pharmacist approx 5% with Hashimoto's are coeliac, but over 80% find gluten free diet helps, sometimes significantly. Either due to direct gluten intolerance (no test available) or due to leaky gut and gluten causing molecular mimicry (see Amy Myers link)
Changing to a strictly gluten free diet may help reduce symptoms, help gut heal and slowly lower TPO antibodies
While still eating high gluten diet ask GP for coeliac blood test first or buy test online for under £20, just to rule it out first
Assuming test is negative you can immediately go on strictly gluten free diet
(If test is positive you will need to remain on high gluten diet until endoscopy, maximum 6 weeks wait officially)
Trying gluten free diet for 3-6 months. If no noticeable improvement then reintroduce gluten and see if symptoms get worse
chriskresser.com/the-gluten...
amymyersmd.com/2018/04/3-re...
thyroidpharmacist.com/artic...
drknews.com/changing-your-d...
restartmed.com/hashimotos-g...
Non Coeliac Gluten sensitivity (NCGS) and autoimmune disease
ncbi.nlm.nih.gov/pubmed/296...
The predominance of Hashimoto thyroiditis represents an interesting finding, since it has been indirectly confirmed by an Italian study, showing that autoimmune thyroid disease is a risk factor for the evolution towards NCGS in a group of patients with minimal duodenal inflammation. On these bases, an autoimmune stigma in NCGS is strongly supported
ncbi.nlm.nih.gov/pubmed/300...
The obtained results suggest that the gluten-free diet may bring clinical benefits to women with autoimmune thyroid disease
nuclmed.gr/wp/wp-content/up...
In summary, whereas it is not yet clear whether a gluten free diet can prevent autoimmune diseases, it is worth mentioning that HT patients with or without CD benefit from a diet low in gluten as far as the progression and the potential disease complications are concerned
restartmed.com/hashimotos-g...
Despite the fact that 5-10% of patients have Celiac disease, in my experience and in the experience of many other physicians, at least 80% + of patients with Hashimoto's who go gluten-free notice a reduction in their symptoms almost immediately.
Getting bloods retested 6-8 weeks after any dose change (or brand change) in levothyroxine. Or after changing to strictly gluten free diet too
Thank you slowDragon for that good advice, do you think it would help if i started on a low dose of t3 ?
No not at this stage
Ft4 is low and a TSH is high
You have plenty of room for dose increase in levothyroxine
All vitamins need to be optimal
Folate is deficient
Vitamin D too low
Come back with new post once you get retested after minimum of 6-8 weeks on 100mcg
You may need further dose increase
Even if we don’t start on full replacement dose of levothyroxine , most people need to increase dose slowly upwards in 25mcg steps (retesting 6-8 weeks after each increase) until on full replacement dose
NICE guidelines on full replacement dose
nice.org.uk/guidance/ng145/...
1.3.6
Consider starting levothyroxine at a dosage of 1.6 micrograms per kilogram of body weight per day (rounded to the nearest 25 micrograms) for adults under 65 with primary hypothyroidism and no history of cardiovascular disease.
gp-update.co.uk/Latest-Upda...
Traditionally we have tended to start patients on a low dose of levothyroxine and titrate it up over a period of months.
RCT evidence suggests that for the majority of patients this is not necessary and may waste resources.
For patients aged >60y or with ischaemic heart disease, start levothyroxine at 25–50μg daily and titrate up every 3 to 6 weeks as tolerated.
For ALL other patients start at full replacement dose. For most this will equate to 1.6 μg/kg/day (approximately 100μg for a 60kg woman and 125μg for a 75kg man).
If you are starting treatment for subclinical hypothyroidism, this article advises starting at a dose close to the full treatment dose on the basis that it is difficult to assess symptom response unless a therapeutic dose has been trialled.
A small Dutch double-blind cross-over study (ArchIntMed 2010;170:1996) demonstrated that night time rather than morning dosing improved TSH suppression and free T4 measurements, but made no difference to subjective wellbeing. It is reasonable to take levothyroxine at night rather than in the morning, especially for individuals who do not eat late at night.
BMJ also clear on dose required
hi, just wondered if smoking has any effect on the thyroid as i have a white patch covering my thyroid! It has been there since my underactive began about 5 years ago, i knw i have hashimotos has you told me. I try real hard to cut out smoking and am down to 5 a day. Any help would be greatful. Many thanks...
Never heard of white patch on thyroid before
Smoking can affect thyroid levels. If/when you eventually stop, test thyroid levels regularly
thank you once again