Reposted blood results
Blood results: Reposted blood results - Thyroid UK
Blood results
jodary
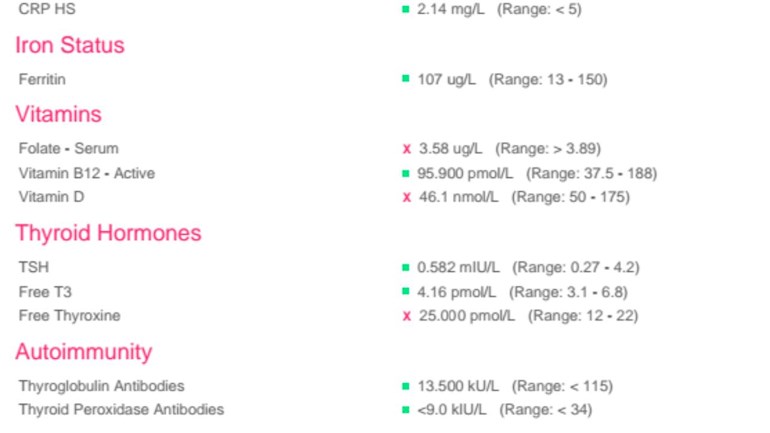
CRP-HS, Ferritin and Active B12 are all fine.
Folate is below range so technically you are folate deficient and should speak to your GP who may prescribe folic acid.
Vit D at 46.1 (18.44ng/ml) is insufficient, some GPs will prescribe a low dos Vit D supplement to achieve a level of 50, but you'd be better off dealing with this yourself.
The Vit D Council recommends a level of 125nmol/L (50ng/ml) and the Vit D Society recommends a level of 100-150nmol/L (40-60ng/ml).
To reach the recommended level from your current level, the Vit D Council suggests supplementing with 4,900iu D3 daily (nearest is 5,000iu).
vitamindcouncil.org/i-teste...
Retest after 3 months.
A good quality D3 supplement at a very reasonable price is Doctor's Best softgels. Check out Dolphin Fitness who are usually the cheapest.
When you've reached the recommended level then you'll need a maintenance dose to keep it there, which may be 2000iu daily, maybe more or less, maybe less in summer than winter, it's trial and error so it's recommended to retest once or twice a year to keep within the recommended range. You can do this with a private fingerprick blood spot test with an NHS lab which offers this test to the general public:
There are important cofactors needed when taking D3 as recommended by the Vit D Council -
vitamindcouncil.org/about-v...
D3 aids absorption of calcium from food and K2-MK7 directs the calcium to bones and teeth where it is needed and away from arteries and soft tissues where it can be deposited and cause problems such as hardening of the arteries, kidney stones, etc.
D3 and K2 are fat soluble so should be taken with the fattiest meal of the day, D3 four hours away from thyroid meds if taking tablets/capsules/softgels, no necessity if using an oral spray
Magnesium helps D3 to work. We need Magnesium so that the body utilises D3, it's required to convert Vit D into it's active form. So it's important we ensure we take magnesium when supplementing with D3.
Magnesium comes in different forms, check to see which would suit you best and as it's calming it's best taken in the evening, four hours away from thyroid meds if taking tablets/capsules, no necessity if using topical forms of magnesium.
naturalnews.com/046401_magn...
Check out the other cofactors too (some of which can be obtained from food).
TSH: 0.582 (0.27-4.2)
This is good.
FT4: 25 (12-22)
This is obviously over range.
FT3: 4.16 (3.1-6.8)
This is 29% through range.
These results suggest poor conversion of T4 to T3. For good conversion we need optimal nutrient levels so addressing the low Vit D and the folate deficiency should be where you start. Supplementing with selenium ( l-selenomethionine or a yeast bound selenium, avoid selenite or selenate) and zinc can help with conversion. It would be a good idea to test them, especially zinc because it needs to be balanced with copper).
After addressing these, if FT3 remains low whilst FT4 is high, then it may be that you need to add T3 to a reduced amount of Levo, or consider NDT.
My gp is wanting to reduce my thyroxine dose again as my t4 is over range. Since xmas its been reduced and then increased again. If its down to poor conversion and vit defiency is it wise to reduce the dose again ?
I have been down the route of over range FT4 with a previous GP, a very long and tedious journey which ended up seeing an endo because my GP was out of her depth, and the endo made things very, very much worse. In the end it was down to nutrient deficiencies and poor conversion, but the NHS didn't recognise this so I ended up helping myself after many years of illness.
As for your over range FT4, to achieve a decent level of FT3 you obviously need a high FT4, but this goes against what GPs have been taught.
Dr Toft, past president of the British Thyroid Association and leading endocrinologist, states in Pulse Magazine (the magazine for doctors):
"The appropriate dose of levothyroxine is that which restores euthyroidism and serum TSH to the lower part of the reference range - 0.2-0.5mU/l. In this case, free thyroxine is likely to be in the upper part of its reference range or even slightly elevated – 18-22pmol/l. Most patients will feel well in that circumstance. But some need a higher dose of levothyroxine to suppress serum TSH and then the serum-free T4 concentration will be elevated at around 24-28pmol/l. This 'exogenous subclinical hyperthyroidism' is not dangerous as long as serum T3 is unequivocally normal – that is, serum total around T3 1.7nmol/l (reference range 1.0-2.2nmol/l).*"
*He recently confirmed, during a public meeting, that this applies to Free T3 as well as Total T3. You can obtain a copy of the article by emailing Dionne at tukadmin@thyroiduk.org print it and highlight question 6 to show your doctor.
Dr Toft has since written a new article which says that some patients benefit from the addition of T3:
rcpe.ac.uk/sites/default/fi...
So you could discuss this with your GP, whether s/he will be open to this who knows. You could point out the past reducing/increasing of your dose of Levo and say that this has not stabilised your levels so it obviously isn't working. A thyroid specialist - as opposed to an endocrinologist who is a diabetes specialist - will want nutrient levels optimal, so the first thing to do is address the folate deficiency and low Vit D and go from there.
Thank you so much. I don't feel at all well as I am and have started having night sweats which gp says is anxiety But this struggle to get well again is adding to anxiety. X
Insist you stay on this dose of Levothyroxine and that vitamin deficiencies are addressed
Improving vitamins will improve conversion of FT4 to FT3
Vitamins are low because dose of Levothyroxine keeps being reduced
B12 and folate work together. Your folate is deficient
Your folate is deficient and this will affect B12
Low B12 can cause night sweats
bmj.com/content/349/bmj.g52...
Low Vitamin D and low B vitamins also interlinked
drgominak.com/sleep/vitamin...
While improving low vitamin D look at also supplementing a good quality daily vitamin B complex, one with folate in not folic acid may be beneficial.
chriskresser.com/folate-vs-...
B vitamins best taken in the morning after breakfast
Recommended brands on here are Igennus Super B complex. (Often only need one tablet per day, not two. Certainly only start with one tablet per day after breakfast. Retesting levels in 6-8 weeks ).
Or Jarrow B-right is popular choice, but is large capsule
If you are taking vitamin B complex, or any supplements containing biotin, remember to stop these 7 days before any blood tests, as biotin can falsely affect test results
endo.confex.com/endo/2016en...
endocrinenews.endocrine.org...
Thank you for this invaluable advice. I think I will try and correct this myself and not consult my gp. Its a new gp and since I started seeing her at xmas my problems have started. I should never have taken her advice. I was actually suffering from anxiety and was quite low. I was probably not overmedicated as she said , it actually was anxiety.
Anxiety and depression are both common hypothyroid symptoms
List of hypothyroid symptoms
thyroiduk.org.uk/tuk/about_...
Yes and I had to refuse antidepressants which would have probably interacted with thyroxine in some way
Unfortunately for me I have just found out that folate can increase platelets and already am being treated for a high platelet count. im not sure where that leaves me now. I am somewhat complicated. But I despair of ever feeling well. I will have to see what they can suggest if anything
According to this website, High platelet count can be due to number different issues,
including iron deficiency Anaemia especially is connected to heavy blood loss......
heavy periods are frequent symptom of hypothyroidism - is that something you suffer from?
I have heard antibodies mentioned quite a lot in determiming if your hypothyroidism is caused by Hashi. Could you possibly give a opinion on my results ? Would appreciate it ,my gp is being unhelpful and wouldn't look at my medichecks results. Said they were irrelevant as it wasn't 12 weeks since I changed my dose back to 100mcg. I am feeling like I am overmedicated now l am so fed up.Thank you.
Those antibody results show negative for autoimmune thyroid disease. They would have to be over range to be positive. If your TPO antibodies were over, say 18 then I would think possibly you may have Hashi's and they were just low at that time.
TPO is the main antibody that confirms Hashi's, sometimes both are positive, but sometimes negative TPO but positive TG antibodies confirm it, but positive TG antibodies on their own can also be due to something else.
One negative result doesn't rule out Hashi's, you'd need a few low results over time, I've had mine tested quite a few times over the years, more recently as part of a thyroid/vitamin bundle, and TPO have generally been between 6 and 11-12. TG antibodies have usually been similar.
It is possible to have Hashi's without raised antibodies apparently, but I imagine you'd experience the fluctuations in symptoms and test results for TSH, FT4 and FT3, that go with Hashi's that would suggest it.
Thank you for your response. im not really clear on what other causes there are. Ive been hypothyroid for over 30 years and on the same dose for that time. of course all those years ago there was not a lot to learn about the condition. Recently my levels have become somewhat erratic which is why I am trying to look into things myself. Am feeling somewhat isolated almost as if the gps arent interested .
im not really clear on what other causes there are
Other causes of hypothyroidism?
Environmental toxins attacking the thyroid.
Failure of the pituitry or hypothalamus.
Adrenal insufficiency affects thyroid working.
Genetic - thyroid gland might not develop properly.
Haemochromatosis where excess iron is deposited in different parts of the body, including the endcrine glands.
Iodine deficiency.
Too much iodine.
Certain medication.
Gladular fever (Epstein-Barr virus)
Major trauma to head, neck, adrenals.
Certain surgery, eg tonsillectomy, gall bladder removal, hysterectomy.
Pregnancy.
(Taken from Dr Peatfield's book "Your Thyroid and How to Keep it Healthy".)
I was diagnosed hypothyroid in 1975 after 2 years of visiting the doctor with symptoms. Back then nothing was explained. I consulted with Dr Peatfield about 20 years ago, in my history he flagged up tonsillectomy aged 5, and the fact that my hypothyroidism started a few months after giving birth to my second child.
It was only when I did extensive tests myself, after many years of being unwell, that I discovered nutrient deficiencies, poor conversion and adrenal problems. Since then I've helped myself because GP not in the least interested, I have optimised my nutrient levels, adrenals are a work in progress but seem to be improving, and I take some T3 with my Levo due to poor conversion confirmed by blood and urine thyroid tests.