I’m pregnant through my first ivf cycle. Went to the doctor as I thought I needed to increase my levothyroxine.
He took my blood to test and said to call back on Friday. I’m not sure if the pregnancy will have put extra demand on my body yet at I’m only 3 week 3 days, the joys of ivf you find out super early! So my blood work won’t so my bodies need for extra meds. I have to retest in 4 weeks if bloods come back fine.
He googled what to do while I was there with him! And said testing now and again in 4 weeks is standard practice. Last time I was pregnant they put my dose up by 25mg straight away without testing.
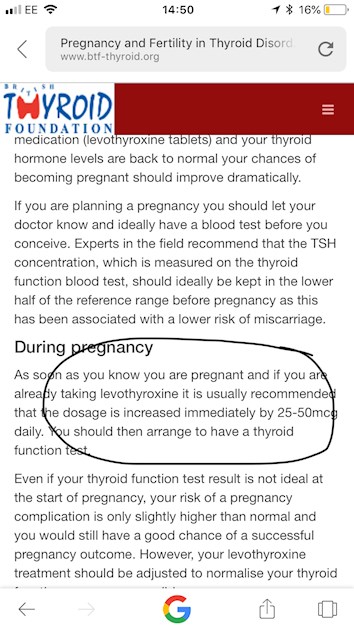
I googled when I got home and the British thyroid society and they said to increase straight away!
What should I do? I don’t want to miscarry again.