One for the midwives!
One of the very first posts on the site when it first started was about the heightened risk of breech positioning in hypothyroidism. The issues keep being reported, keep being experienced, and very sadly, keep being ignored.
Aust N Z J Obstet Gynaecol. 2013 Oct 1. doi: 10.1111/ajo.12131. [Epub ahead of print]
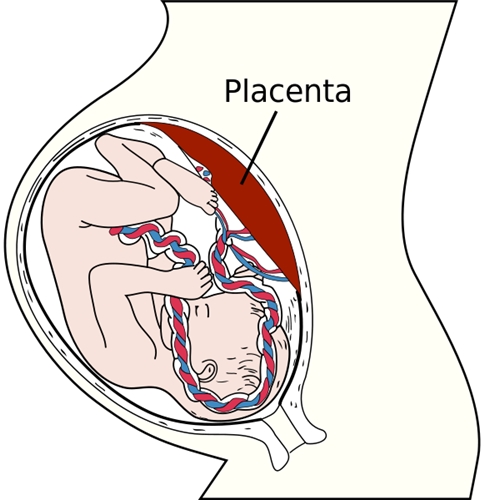
Subclinical hypothyroidism as a risk factor for placental abruption: Evidence from a low-risk primigravid population.
Breathnach FM, Donnelly J, Cooley SM, Geary M, Malone FD.
Source
Department of Obstetrics and Gynaecology, Royal College of Surgeons in Ireland, Dublin, Ireland.
Abstract
BACKGROUND:
Subclinical thyroid hypofunction in pregnancy has been shown to have an association with neurodevelopmental delay in the offspring. It is unclear whether obstetric factors may account for this observation.
AIMS:
To establish the prevalence of subclinical hypothyroidism (SCH) in a low-risk primigravid population and to explore its association with obstetric sequelae.
MATERIALS AND METHODS:
Nine hundred and fifty-three primigravid women had thyroid hormone indices analysed in the early second trimester. Delivery and neonatal outcomes were available for 904 women who met the criteria for inclusion in the study. Women with subclinical hypothyroidism (thyroid-stimulating hormone (TSH) values at or above the 98th percentile with a normal free thyroxine (fT4)) or isolated maternal hypothyroxinaemia (fT4 level at or below the second percentile with a normal-range TSH) were compared with biochemically euthyroid controls. Chi-squared test and analysis of variance were used for statistical analysis.
RESULTS:
The prevalence of SCH or isolated maternal hypothyroxinaemia was 4%. Positivity for antithyroid peroxidase (TPO) or antithyroglobulin (ATG) antibodies correlated with SCH status (P = 0.02). Placental abruption was observed more commonly in the setting of either SCH or isolated maternal hypothyroxinaemia when compared with euthyroid controls (P = 0.02 and 0.04, respectively).
CONCLUSIONS:
Subclinical hypothyroidism and isolated maternal hypothyroxinaemia are associated with placental abruption. The observation of these effects in this healthy low-risk population lends weight to the case for antenatal screening for diminished thyroid reserve.
© 2013 The Royal Australian and New Zealand College of Obstetricians and Gynaecologists.
KEYWORDS:
placental abruption, subclinical hypothyroidism, thyroid autoimmunity
PMID: 24111733 [PubMed - as supplied by publisher]
ncbi.nlm.nih.gov/pubmed/241...
Rod