Ask an ovarian expert anything. Join the conversation by replying to this post.
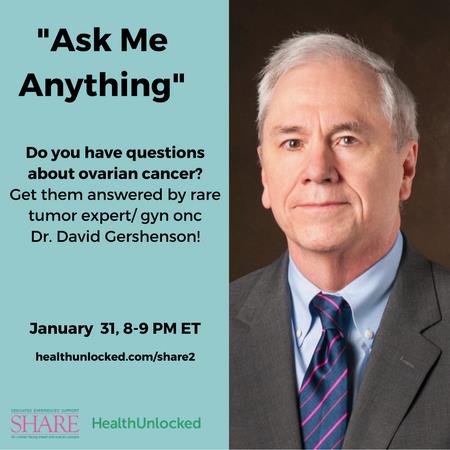
Our Ask Me Anything (AMA) with Dr. David Gershenson is starting now.
We recommend that you click the “Follow Post” button directly underneath the official post and next to the “Like” button so that you will receive notifications of what questions have been posted and what the replies are, in case your question has already been asked by another member. In order to make sure that you are seeing the most up-to-date questions and answers, you will need to continue to refresh your browser to show all of the replies.
At 9pm, at the end of the AMA, we will lock the thread, so that no more questions can be posted in the thread. If you miss the AMA, we will keep the post on the community so that you can see all of the questions and answers from the session!
Guidelines for Ask Me Anything (AMA):
1. While we always strive to provide useful, up-to-date information on ovarian cancer, the information posted in this Ask Me Anything session should not be used as a means of diagnosis or determining treatment. For diagnosis and treatment options, you are urged to consult your physician.
2. Please try to keep questions general, and not overly specific to your personal clinical situation. We want these questions and answers to provide useful information to the entire community.
3. Please try to limit your questions and responses to three sentences.
4. As always, please be respectful of other members and their questions.