Hi folks; sons b12 was 174 (130-800) his b12 active is 33pmol/l (25-108) his MMA is 265nm/l (0-280) any adv would be great, got GP apt on 7/4/17. Family history of PA incl Mother and Grandfather. X
Update on 18 yr old son: Hi folks; sons... - Pernicious Anaemi...
Update on 18 yr old son
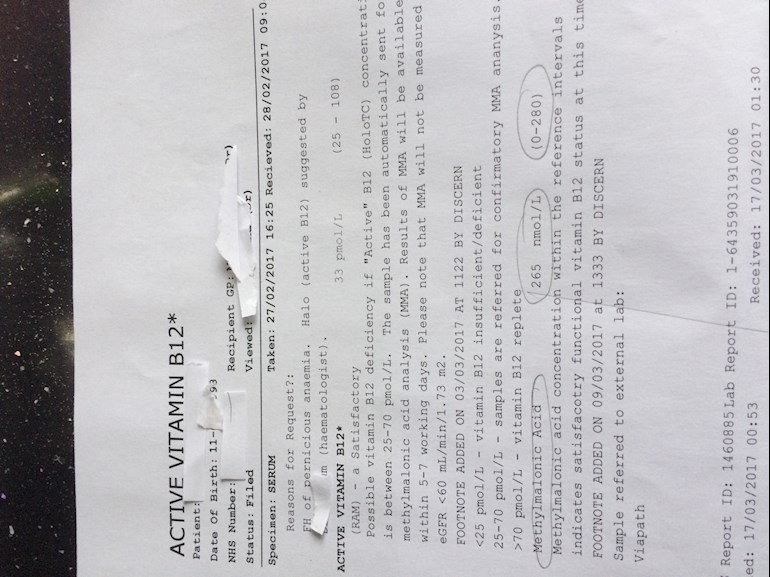
Its one indicator and its pointing away from B12 deficiency at the moment - though doesn't mean that it isn't bubling away. active B12 is in range as well.
Sorry but I can't remember how symptomatic your son was.
Have you ruled out other possibilities for the symptoms, such as thyroid?
Hi Gambit, don't know if Ferritin and folate have been checked. He was diagnosed with Gastritis in Dec 16.... he's also breathless and fatigued at times.
Gastritis can affect absorption of B12 and a lot of other vitamins.
Evaluating B12 deficiency is a tricky thing and I'm definitely not saying that your son doesn't have a deficiency - just that the holo-T and MMA aren't backing necessarily backing up the serum B12 being low - and I'm not sure what ranges GP is used to dealing with - some labs have lower ranges even with the same kit.
iron based anaemia would cause breathlessness and fatigue. Have you managed to get hold of tests that the GP has done.
iron based anaemia would also make it harder to interpret full blood count as it will tend towards micro rather than macrocytosis.
Suggest that you try to get hold of copies of any blood tests GP has done, and try putting things in writing to GP and then follow up with an appointment. I really hope that you can get GP to think beyond test scores and if iron isn't showing up/gets ruled out as a cause then hope that he will agree to trialling B12 in the absence of any other possibilities,
Hi SarahFerguson.
I note that it states on the blood test results you've posted 'possible B12 deficency if active B12 concentration is between 25 - 70pmol/L. An active B12 level of 33 pmol/L puts his result towards the bottom of that range - and as the lab states, this does suggest a possible B12 deficiency (your GP may just look at the results and fail to spot the specific qualification about deficiency levels added by the lab).
And you're right, with his previous serum B12 level of 174, he should be diagnosed with antibody negative PA - as per BSCH Guidlines - and especially because of the family history of PA.
Also - he has neurological symptoms so should be treated with the intensive neurological regime of injections (6 x loading doses on alternate days and the injections every other day until no further improvement). Your GP may not know about this regime - it's in the BNF - the doctors prescribing bible - he'll have a copy on his desk and can look it up. It's the second items down so he'll have to look further than usual.
Be aware - the BNF treatment guideline states that this is the treatment for PA so some GP's refuse treatment if PA is not a confirmed diagnosis. This is wrong. What the BNF fails to say is that the treatment for PA is the treatment for the B12 deficency it causes. B12 deficency has other causes too and the treatment for B12 deficency, PA or otherwise, is the same: B12 injections. (Just to give you the heads-up 😄).
Can't remember if I've left you links to information and guidelines before (shout if not and I'll post them for you) but here's a link to a document that may help you to get treatment for your son. It's a UKNEQAS B12 Treatment Alert which advises medics that neurological symptoms associated with B12 deficency should be treated immediately to prevent possible neurological damage, even if serum B12 levels are within the 'normal' range. You have two results, one of which the BSCH guidelines say should be treated (as antibody negative PA) and the other which a lab advises as within the possible B12 deficent range. It should not be beyond the wit of your GP to put two and two together, consider the neurological symptoms, and get out the B12 injections.
Here's the alert:
onlinelibrary.wiley.com/doi... (UKNEQAS B12 Treatment Alert, Neurological Symptoms and Risk of Subacute Combined Degeneration of the Spinal Cord)
About the MMA - it's towards the top of the range but not out of range. This could be indicative of declining B12 levels - but your GP will say it's normal.
Also agree with gambit - your GP should check ferritin (a marker for iron deficiency anaemia) and folate levels. B12 and folate work together so if folate is deficenct or low in the range then the body cannot utilise B12 properly.
Also (and sorry, can't remember) has your son had an FBC blood test? You can post results here for help,with interpretation (GP's often say things are normal when they're not). If one hasn't been done, it'd be a good idea to ask your GP to do one.
Also - and a passing / parting thought...gastritis can often be an early symptom of PA, which progresses through several stages (four, I think) until Autoimmune Metaplastic Gastric Atrophy (PA) becomes fully developed.
Anyway SarahFerguson, very best of luck with your GP appointment...let us know how you get on and post again if,you need any help prepRing for,your appointment (sounds like you've been preparing already 😄😄).
👍
Thank you all so much, I am thinking that he's developing PA, but at the early on-set hence results showing inconclusive, but something is definitely going on! The GPS are having a look at my sons case as the surgery is a partnership. I will be asking for FBC and Ferritin / Folate blood tests when I see them on Friday. Thank you all again x