We’ve seen some discussion of EPO levels and PV Dx. I am one of the members who has an unspecific mix of ET/PV and curious about EPO. I found a related report.
Quick summary of the report:
-Low EPO is not unusual in ET
-Low EPO ET has lower MF transformation
-Low EPO ET has higher PV progression
-Low EPO has higher thrombotic risk
For reference the 2016 WHO PV Dx criteria are shown at the end of this post. EPO is a minor part.
In this report “Serum erythropoietin levels in essential thrombocythemia: phenotypic and prognostic correlates” there is various new info to me on some prognostic items. As always this is just one report, we’d need multiple such reports to have more certainty. Other references/comments are welcome
ncbi.nlm.nih.gov/pmc/articl...
They studied patients without any cytoreduction and I think they did not receive any during the evaluation period. EPO levels were low in 62 of 177 confirmed ET patients. So low EPO does not preclude ET, consistent with EPO being a minor criteria for PV.
WBC median was normal-high in these ET patients with upper ranges being in the 20’s, well over normal, so WBC can also be abnormal in ET.
PLT was high, not a surprise.
-Is BMB required? ->According to the WHO, for PV you can skip the BMB if you are Jak2, your Epo is low and H/H is constantly very high (18.5/55.5% Male, 16.5/49.5% Female) So EPO matters here for PV Dx. But per WHO if your H/H is just a bit high you need BMB to be sure of PV Dx.
--
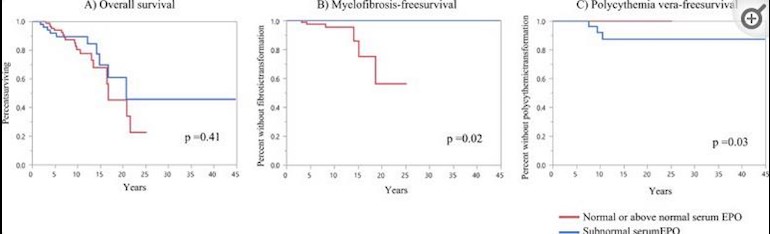
Implications of low EPO in ET: See plots for events vs Epo levels.
-Most striking is low EPO was correlated to MF free survival, zero transformations for low EPO.
-PV transformation was equally extreme but opposite, being zero for high EPO.
-Thrombotic risk was higher for low EPO.
-Survival was similar for each, but this P value (statistical significance) was not good at 0.41, so the MF and PV events are more reliable results.
-Leukemic transformations were low and similar, but as above P value is also not good. Low P values are likely because there were too few such events.
My thought is if these pts had cytoreduction (HU, INF) at least the thrombotic risk would be much less as we’ve seen in other discussions.
By the WHO criteria and in context of this report, my amateur opinion has me with ET, but I won’t argue with Dr’s Dx.
--
Major WHO criteria requires the presence of either all three major criteria or the first two major criteria and the minor criterion
1. Hemoglobin >16.5 g/dL in men and >16 g/dL in women, or hematocrit >49% in men and >48% in women, or red cell mass >25% above mean normal predicted value
2. Bone marrow biopsy showing hypercellularity for age with trilineage growth (panmyelosis) including prominent erythroid, granulocytic, and megakaryocytic proliferation with pleomorphic, mature megakaryocytes (differences in size)
3. Presence of JAK2V617F or JAK2 exon 12 mutation
The minor WHO criterion is as follows:
· Serum erythropoietin level below the reference range for normal
Criterion 2 (bone marrow biopsy) may not be required in patients who have sustained absolute erythrocytosis (in men, hemoglobin/hematocrit of >18.5 g/dL/55.5% or in women, >16.5 g/dL/49.5%) if major criterion 3 and the minor criterion are present