TAKE-HOME MESSAGE
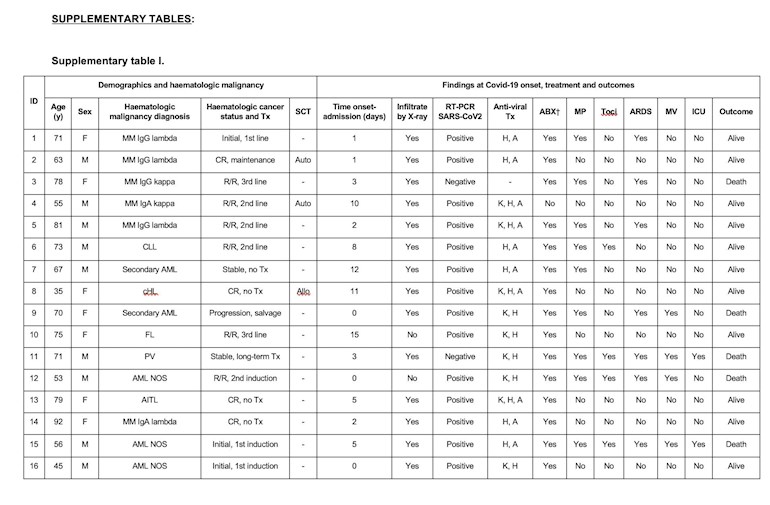
This retrospective cohort study evaluated outcomes in 34 patients with COVID-19 infection and concurrent hematological malignancies. Patients were stratified into survivors (n=23) and non-survivors (n=11) for comparative analyses. On review of baseline clinical and laboratory parameters at illness onset or on admission, only procalcitonin levels were significantly higher in non-survivors than survivors. The development of acute respiratory distress syndrome, an ECOG performance status ≥2, and qSOFA score ≥2 were associated with shorter survival.
This cohort study describes the presenting clinical and laboratory characteristics in a diverse group of hematological malignancy patients admitted with COVID-19 infection and provides data on outcomes in this vulnerable patient population.
– Curtis Lachowiez, MD
The prevalence of cancer in patients with the novel coronavirus disease 2019 (Covid-19), caused by the SARS-CoV-2 infection, is uncertain. In a pooled meta-analysis including 11 retrospective studies, the prevalence of cancer was 2% (Desai et al, 2020). Patients with cancer and Covid-19 have been described to have a higher risk of suffering severe events (intensive care unit admission and invasive ventilation or dying) in a retrospective study including 18 patients with cancer (Liang et al, 2020). One study reported 13 Covid-19 cases in a cohort of 128 hospitalized patients with haematological cancers, with no significant differences in baseline co-variates between patients developing or not developing Covid-19 (He et al, 2020).
practiceupdate.com/C/100506...
(Could only attach one photo of the table data, but essentially there were 3 PV patients of the n=34....none of them made it :(....though they were 71, 85, and 94).