Why didn't I read this earlier?!
Really helped me. Someone on here, maybe Cecily p... - LUPUS UK
Really helped me. Someone on here, maybe Cecily parsley? Said she'd read all of the books. Thank you.
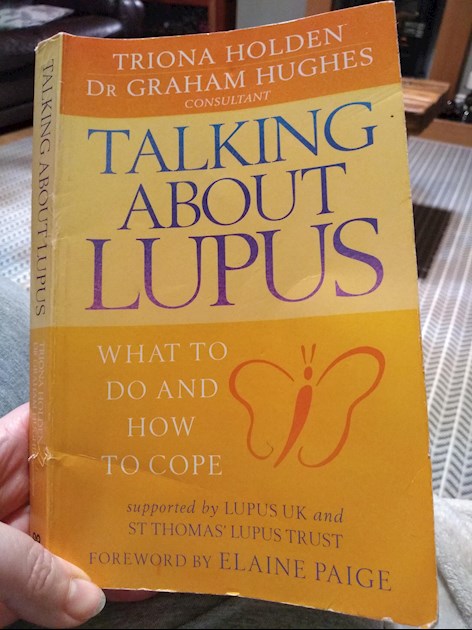
2004 I'm now wondering if there's a more recent one x
I haven’t read that one Bonny but I read one by Graham Hughes when I was first diagnosed 8 years ago. It really helped! I don’t know if there are more up to date versions but I did recently listen to a lecture by Professor Hughes given in Melbourne which I found by Googling him. He is definitely the expert and such a caring sympathetic man with it. Hope this helps. 🤗
Oooh this looks great! There are a number of really good (but sadly very expensive) books out there. I've started reading clinician guides - mainly because my treatment has been so bad since I came home so I wanted to know what best practice is in terms of frequency of appointments, regularity of tests (and which tests), medication and what to watch out for. So at least I can advocate for myself in the face of a hostile/disinterested rheumy.
These are the books I'm currently reading but they are pricey... I'm lucky as I've managed to access them for free through my former university's online library.
springer.com/gp/book/978146...
springer.com/gp/book/978190...
springer.com/gp/book/978184...
In the first book I list above, it describes precisely what my treatment was like when I lived abroad - rheumatologist available on email/phone in emergencies etc. This is what it says on page 53:
"Effective patient care entails the development of a trusting relationship and workable
treatment plan between patient and physician. Clear mutual goals should be set
whose basic aims are to alleviate symptoms, prevent exacerbations, treat relapses,
prevent permanent organ dysfunction, and prevent damage from treatment. Probably the most important part of a successful long-term treatment program for
the lupus patient is the development of open communication and a sense of trust
between patient and physician. To the physician, this means not only regular office
visits with time for discussion, answering questions, and offering explanations but
also availability for emergencies (e.g., by telephone and e-mail).
Patients with lupus are confronted with the unknown, a potentially disabling
chronic disease and at times the fear of dying. The patient may have seen a definition
of lupus on line as a “fatal disease of young women.” Patients with lupus need reassurance,
sympathy, support, and frank discussions, not just initially but on subsequent
visits, regarding their disease as well as the stress the disease puts on them."
Don't settle for less my lupus friends!! I've said it many times, but I'm really shocked at the standard of care here at home in the UK and I really really hope Lupus UK and all the other wonderful advocating academics we have help take us closer to where we should be. Good care not only will help us avoid the absolute worst outcome but also could keep us healthier for longer reducing the burden on the NHS. The current state of medical care being given literally isn't just bad for us it's bad long term for the NHS. Proactive preventative care could keep us healthier easing the burden on the NHS. It's a no brainer and the clinician guides really lay out what good care looks like, so there's no excuse to not be implementing this for all of us.
Another amazing quote on p54:
"The physician should educate the patient with regard to signs suggesting that the
disease is becoming more severe. These signs include malaise, poor appetite, weight
loss, weight gain, fatigue, pallor, irregular and heavy menses, fever, arthritis, seizures,
cognitive abnormalities, mood changes, difficulty coping, chest pain, edema,
excessive hair loss, oliguria, rashes, and mouth sores. The physician should routinely
ask about these signs at each visit and encourage patients to bring in problem/question
lists. In some instances these symptoms have causes other than lupus and should
be investigated and treated. Patients often become anxious regarding the interpretation
of laboratory tests. Explanations of test rationale and results are helpful.
Often patients are more concerned with the side effects of medication than with
their benefits. The physician should monitor for drug allergies; drug interactions,
whether medications should be taken prior to, with, or after meals; and medication
cost.
The physician needs to focus not just on prolonging life but also on improving
the quality of life."
Oh thanks. I'm not sure I'm ready for the stage you're at yet. I found it to be like an introduction. I'll take look when I have more time and experience though, thank you x
Insomiacette, The excerpts you chose to share should be framed in every doctor's office. I am in the Us, and it seems that doctors are getting less and less focused on patients as people, but see us as lab results at one given moment. We leave an appointment with little or no validation of what we are experiencing and emotionally, feeling worse.
Healing hugs.
Hugs back at you Pumpkin2009.
So what I'm going to do is go through the clinician's handbook on both Lupus and Sjogren (as I have both) and work out what I think needs to be done with me. IE how often I think I should be being seen (the book says every six months for people with mild symptoms which is me at the moment), the blood tests that should be done and how often and what I'm concerned to keep an eye on. I'm going to make a list and the next time I go see a rheumy (I'm currently hoping to be sent to a new one soon) I'm going to explain what I've been up to and start the first discussion with my rheumy on what the care plan is for managing this beast so I stay healthy long term and he/she sees me as little as possible.
Obviously if they think I don't need things and can explain why I'm happy not to have blood tests done - for example I have sticky blood and abroad I was tested yearly and sent to a cardio, I also used to see a dermatologist for the lesions on my back and head once every 6 months - I've not seen anyone or been referred to anyone since I've been back to the UK - largely because my rheumy has ignored me totally and not even performed a physical
So... new rheumy new plan. I'm going in with what was happening abroad, backed with the knowledge of what is best practice from the clinician handbooks and starting the discussion from there.
Basically I'm trying to get informed so I can be proactive about my care. Empowered is the word I'm aiming for.
It's a bloody shame I need to do this, but if this is what it takes then this is what it takes...
Huge supportive hugs to you Pumpkin2009!
Insomniacette, Thank you so much. Right now, I am waiting for lab results from my PCP. I just had labs done a week ago from my rheumatologist showing lower anemia and low lymphs, but my PCP wanted his own tests. Because I got Covid early Nov. and still have lingering symptoms, there is definitely confusion of what is lupus and what is Covid. Truthfully, I don't think there is a way to separate symptoms right now other than the lack of taste. That one is definitely Covid. I am now having rib problems on the right side with times of devastating pain which could be either. I am not a pessimist by nature, but feel at this point along with other problems, there aren't going to be concrete answers and not really anything to help with the symptoms, some of which overlap. The rheumatologist did say that it is hard to know at this point what is what. I already realized that not just now, but always because of overlapping conditions. No one seems to just have lupus all by itself. it likes to have friends:).
I like your approach to things and appreciate you knowledge and incite.
Thank you.
No sorry not me Bonny. This looks good though. When I was first diagnosed I read several on the Lupus U.K. list including one on APS. Xx
Please don’t apologise I mix people up all the time. I am really pleased someone did the reading and helped you with recommendations xxx