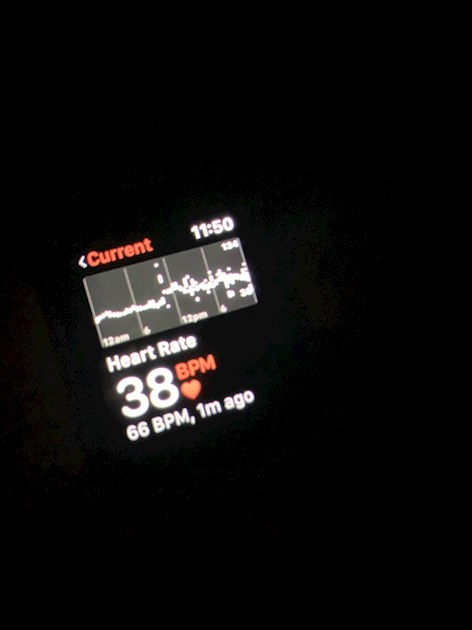
Hi I’m currently waiting to see a cardiologist but there is up to an 18 week wait, I went to my doctor because I was worried about my heart rate. I felt a bit off one day at work and the the nurse checked my obs (I work in an inpatient unit) and my pulse was 42 but the shit up to 128bpm without me even moving. I am no way an athlete I am slightly overweight which I am currently sorting. Since then Iv noticed it get worse, I get a tight chest, I don’t gasp for air but I have to take deep breaths until this passes! I now have an Apple Watch so I can track my heart rate and it goes off most nights because my pulse is low, it even goes down to 38bpm! I was just wondering what people’s opinions on this was as there is an 18 week wait, or any suggestions on what I can do? Thank you, Sophie 
Heart rate, opinions : Hi I’m currently... - British Heart Fou...
Heart rate, opinions
I think you should definitely keep an eye on your heart rate and record it whilst you wait for an appointment.Of course, if your heart rate becomes excessively slow or fast in the meantime you may need to seek medical help sooner.I'm sorry it is such a long wait.I had a similar wait to see a cardiologist for a different reason but once you are in the system things should improve.
You are symptomatic at times so that's a bit concerning.
I would call and let the md know what's been going on.
Let the md decide what should be done.
It's good you work in a place you can be checked. Can they do an ekg when you have symptoms?
That tracing from your watch looks like artifact to me. It could just be because I'm on a phone. But if you can get some good tracings of what your heart is doing when you have the symptoms it would be great to show the md.
Hi you are lucky I have waited 5 months to see my cardiologist. Would have longer but k wrote to him in October and finally got a appointment for January
Good luck
18 weeks is just two weeks less than 5 months!
As already said - go to GP and let them have your recordings. Please remember that smart watches can be very unreliable, especially at night due to connectivity to the skin that can cause false reading. Have you heard of white coat syndrome?
What is white coat syndrome do tell please
What does your GP say about your heart rate? Are they concerned.
Hi Sophie
Quick question is do you take any medication ?? and is it an erratic pulse you have been referred to a Cardiologist for checking ? My understanding is a Low Pulse in it's self is not something to be over concerned about unless it is causing you problems. As people have said you can keep a record of Highs and Lows so you can tell your GP or Cardiologist, I believe it's quite important to record any symptoms at the time..
Don't forget if you feel unwell through any of this A & E is always a route to take !!
Regards
My resting pulse is in the low 40's and can drop to high 30's during sleep. I'm 56 and while reasonably fit for my age I'm no athlete. I have additional ectopic beats that don't register with Fitbit, applewatch etc.... an ECG will pick these up. I've probably been like this for several years but it was only picked up about 18 months ago as part of a routine check up for my rheumatoid arthritis, I was then referred to a cardiologist. My heart rate is still low, but my Cardiologist is less concerned about this than other symptoms, like breathlessness, water retention, chest pain. It has limited the dose of beta blockers I can take to try and address the ectopics but other than that it seems to have little impact day to day. It probably contributes to general tiredness though, I guess.
Disclaimer: I am not medically trained, just a patient with decades of personal experience.
Given you're reporting in your post that you're now experiencing chest tightness requiring you to deep breath for relief, I think you're best served telephoning your GP (who presumably is the referral point to the cardiologist) and reporting the new symptoms.
When I reported something quite similar my GP ranked it as 'chest pain' and I was fast tracked to the Rapid Access Chest Pain unit - I was seen at the RACP unit less than two weeks after reporting the chest tightness and shortness of breath. Further investigations followed rather quickly after the initial RACP appointment.
If I hadn't been fast-tracked I'm not sure I would still be here - my chest tightness was my body's way of telling me and the GP my recurrent pericarditis was in an acute flare, and further investigations showed pericardial effusion that had to be monitored and medicated to prevent cardiac tamponade (a life-threatening complication I've been through a few times and no it is not fun).
It depends on your GP deciding yes/no regarding the urgency of your new symptoms and if he/she decides your description of 'chest tightness' meets his/her criteria for 'chest pain', and sadly it also depends on your location - if your trust is overloaded with patients going through 'crippling pain' level symptoms, you might be shuffled to the back of the queue.
But your GP should know about these new symptoms and take any fast-tracking decisions. I'd telephone first thing tomorrow morning. Please update us soon as - we'll be thinking of you until we hear back!
Hi all thank you for your replies. When I went to the doctors I told him everything about the tightness in my chest, dizziness and shown his the recordings from my watch. My pulse was low In the low 40s when I seen the nurse a few months ago and he didn’t seem to bothered really just referred me. Since Iv become aware of this I have been noting symptoms when they happen. I don’t really notice when it drops always it’s more when it comes back up I get the right chest etc. I don’t take any medication at all either. My pulse doesn’t always drop to high 30s when I’m asleep it does it in the day also stays in the low 40s for a short time and then jumps back up.
Periodically ring the hospital and ask if there are any cancellation appointments available.
Good luck
Hi
I have recently been diagnosed with Hyperadrenergic POTS, probably, more tests to follow. I am 57 but have had the symptoms you describe for very many years and not really been taken seriously because my BP was always normal, HR fairly normal when sitting. It may be worth taking your HR and BP 10 minutes rested lying down, then stood up at 2 minutes, 5 and then 10 minutes. Have a look at dysautonomia international and POTS UK. The hyperadrenergic variety is POTS with an overshoot of noradrenaline and tends to see large rises and falls so you can get the extremes. There are other dysautonomias which is why i suggest having a look at the dysautonomia site. One is purely Cardiac dysautonomia, or hyperadrenergic heart without POTS. There is a variety.
However, non show structural defects of the heart or damage of the vascular system, or very little because they are an autonomic dysfunction so often get missed.
The breathlessness and pain can be attributed to the massive rises and falls in either BP or HR, so I am told. The nerves around the aortic arch and carotid arteries are very sensitive and the main baroreflex receptors that control how levels and need are situated there. If there is any confusion, the messages to increase or decrease breathing for oxygen levels can get confused.
If its POTS, or another dysautonomia it will very often show itself via a tilt table test that your cardiology centre can do, however, if you find that you have a possible autonomic dysfunction by checking yourself, proper BP cuff needed, your watch will only do a basic HR result, then its worth asking your GP again and take the NHS leaflet for POTS along with you. You can print it out on choices, it suggests you do. A rise of HR 30 when standing, after 10 minutes, sustained or HR 120 sustained, from lying, is a POTS diagnosis, if BP roughly stays the same its confirmed. If it drops it may be one of the sub types or if it rises it is likely to be hyperadrenergic, too much noradrenaline being released.
Dysautonomia is a another option worth exploring  Good luck
Good luck
Try and get some regular gentle exercise on a level path for a round trip of about a mile, preferably with a friend or companion. Keep track of your progress and produce a body of evidence for future reference.
Hi everyone, I ended up in a&e and after an ecg been diagnosed with bigeminy awaiting more tests x