After a year undetectable on Orgovix and Xgeva What are my options now? If second generation meds are needed, which has the least side effects? Xofigo? Pluvicto? Provenge?
Looks like I've gone castrate resista... - Advanced Prostate...
Looks like I've gone castrate resistant. How much trouble am I in?
Forgot to mention that I have a new PSMA scan scheduled for 12/06/22 at City of Hope
You might discuss adding abiraterone or enzalutamide to Orgovyx.
Thanks TA. That seems to be the standard choice for secondary meds. But I don't like the idea of taking prednisone for the side effects. What about Nubequa?
That's a frequent misunderstanding. The dose of prednisone only replaces the cortisol lost by taking Zytiga. It does not add extra corticosteroids beyond what one should naturally produce.
The only second-line hormonals approved for metastatic castration-resistant PCa are abiraterone or enzalutamide.
Thanks again. So that would be Zytiga or Xtandi? Nubeqa would not work or it's not covered by insurance?
Usually not covered. I suspect that apalutamide is the best of them, but that is only a guess.
Is Apalutamide covered?
Not ordinarily. Sometimes MOs can convince insurance to cover it or darolutamide.
I agree with Tall Allen on this. I have been on Lupron and Abiraterone with 5 mg Prednisone and have no additional side effects. The SEs come from Lupron. Blood work is good as well. Just my experience.
Nubeqa is actually available, whether it be for both mCRPC or CRPC, it all depends if the MO will be willing to submit to insurance "medical necessity"... But FDA approved non-metastatic CRPC. What's to lose if you try it a few months and there's a response, or not? And some states have the "Right to Try" laws... So it all depends. Having an aggressive MO in your corner is worth it's weight in gold too! Someone who would fight for your care, not just deflect because the FDA says so. Lol
Nubeqa by trial result, has shown the least impact side effect wise as compared to the other *lutamides. Does that mean it's also less effective? I've always wondered about that, but suspect it may be an individual case basis (heterogeneity).
What's hard to find is correlated data for Darolutamide vs Abiraterone... And difficult even more so to try and determine which might be best to add to the normal ADT as 2nd line. But Darolutamide is the newer of the *lutamides, is it better? Who knows...
I recently began Daro over Abiraterone, as a choice. When I asked my MO about it over Abi, he was all for it, but noted insurance might not approve it. I was ok with that and told him to submit and let's see, not worry about the insurance until we needed to, and if disapproved, we could circle the wagons and go from there.
First prescription I've ever signed for... Lol
Guess the $16k per month isn't something they'll leave on the doorstep! We shall see if it has the desired effect.
All the best!
I am on Xtandi and with approval of my local pharmacy it is delivered there for me to fetch. Safe, reliable. No chance of porch theft, left in sun or cold at my doorstep, no problem while I am away from home for day. No need to adjust my personal life for signature delivery. When I go to he pharmacy I never drive anywhere afterward but home. Too much risk that something would happen during the continued journey.
aberaterone seems to work well for most of us.
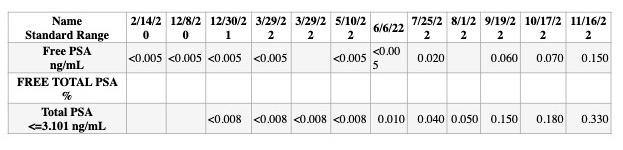
Your PSA doubling time is about 2 months now.
My MO would recommend AA plus Prednisone.
I would personally get Provenge if I could get it as soon as possible, but my MO don't recommend Provenge plus it is not available in Australia.
You are not eligible for Xofigo as you don't have bone pain plus Xofigo infusions would not be helpful with your cancer. You had enough local therapies in a form of radiation.
Maybe you could try again SBRT of your mets if the RO recommends it. (If it is possible safely irradiate your mets. This time don't make a mistake not to use a global therapy.
My idea is that ROs like to see how effective was the SBRT on you by watching how your PSA drops without additional global therapies. That is only to satisfy their medical interest and to learn about the dose etc.
It is not in your interest not to use system therapy just to let them learn on you.
I realized that it is a very common excuse that they are keeping the drug in reserve. Actually they just want to see how the medical procedure what they administered to you is working.
Either it is a simple SBRT, or Lutetium 177 PSMA infusions or Actinium 225 PSMA therapy etc.
I don't believe that I would do Lutetium PSMA therapy at your low volume cancer. It could be simply too toxic to you (kidneys etc) and ineffective.
Plus you have to know that in your lifetime you could only get 6 infusions of radio ligand like Lutetium177 or Actinium 225.
For bone mets Pluvicto (Lutetium 177) is not effective. Maybe you could come to Australia Sydney and take part in a clinical trial with Actinium organized by professor Emmett.
I would not rush in your situation with any radioactive system therapy at your early stage.
Just do Provange and Abiraterone plus Prednisone.
Later above PSA 5 or even better 10 do a liquid biopsy.
Maybe you could at that stage use Olaparib for 2 more years if you develop BRCA genetic mutation.
After that maybe Keytruda, but all of this is far away for you.
I am not a doctor just my opinion.
If you start Abiraterone plus Prednisone you could add Apalutamide later if Abiraterone plus Prednisone are not enough.
I wish you all the best.
István
1. So you think Provenge is effective?
2. At what point would you add it to the mix?
3. After or before second generation med?
Dr. Steinberg at UCLA is my RO and a big believer in SBRT so he will likely want to use that depending on the outcome of my upcoming PSMA scan.
SBRT if it is possible to be administered safely is better for you then Lutetium or Actinium PSMA treatments.
If you use PSMA therapy then you will most probably lose your ability to follow the progression of your PSMA avid prostate cancer on the PSMA PET scans in the future. In that case you will not be able to detect early your mets in order to safely SBRT them.
I believe that Provange is the most effective when it is administered early while your PSA is low, definitely under 5.
Again I am only a hobby oncologist therefore better if you just rely on the guidance of your great university UCLA.
But it is a common knowledge that Provange is most effective earlier ruther than too late.
My MO doesn't recommended it as it doesn't lower the PSA and it would be for me 120k $ what I don't really have in order to extend my life for 4 months.
If you are serious to extend your life I would jump into Provange as soon as possible and the beauty of Provange is that it could be administered parallel to docytaxel chemotherapy.
I really don't know enough about your medical situation to make decisions for you.
I believe that the great UCLA oncologists have all your details on record.
If I were you I would definitely try to consult Dana Farber cancer institute in Boston if for nothing else than for a second opinion. You can initiate the second opinion from Dana Farber cancer institute through the internet. I am thinking here about a second opinion from Dana Farber cancer institute RO. As tango65 already said radiation therapy is a serious business therefore better if you ask for a second opinion from Dana Farber cancer institute radiation oncologist.
"SBRT if it is possible to be administered safely is better for you then Lutetium or Actinium PSMA treatments"
Sbrt is a different animal than the other two treatments.
Sbrt can only treat points. The other two are global treatments.
Sbrt may be a supplement to psma treatments but not a replacement.
You have to be also realistic that at his low PSA levels of 0.3 you don't really have a moral right to poison him at this stage with Lutetium 177 PSMA infusions which is most probably ineffective for bone mets or with Actinium 225 PSMA treatments especially if his PSMA PET scan in December will not show wide spread mets. By targeted killing of the CRPC sports with the SBRT and relying on the immune system to mop up the rest. Provange would be really beneficial plus chemotherapy if his MO will recommend it.
I don't want to bring that link from the Bonn University Hospital about the possible toxicity of the Lutetium PSMA therapy on low volume cancer. Everything should be considered in context. We are not MO s therefore we can't decide, but still we can think high level about the treatments goal.
For bone mets, Pluvicto is not effective?
Isn’t that exactly what most of the patients being treated with Pluvicto have? Wasn’t an outcome measure in the Vision trial “radiographic progression free survival”? So wasn’t it primarily looking specifically at no progression of bone mets?
I am confused. Can you cite a source? There must be some aspect I am not understanding.
I am not a doctor just saying what I see here. I always thought that Pluvicto is for lymph nodes and soft tissue.
I really don't know. You could find this out from your MO?
Xofigo is for bone mets,
Thank you for your reply. Pluvicto is indeed for bone mets.
You repeated it several times in this thread, so I thought perhaps you had seen some recent study.
Both my husband and my brother are receiving Pluvicto for bone mets, so I was worried. I believe you misinterpreted something you may have read.
I am in no way suggesting Pluvicto is appropriate for the original poster. I was just startled by your statement!
I can understand you fully. The problem could arise with the diffuse bone marrow infiltration with a Betta particle emiter (Lutetium).
Other criterium which could eliminate patients for Lu 177 PSMA treatment is diffuse bone marrow infiltration in a PSMA PET/CT.
If these patients are treated with Lu 177 PSMA, many normal blood cells in the bone marrow could be affected by the radioactivity of the Lu 177 PSMA attached to cancer cells in the proximity and make the hematological problems even worse.
The bone marrow of these patients could be affected less if they are treated with Ac 225 PSMA since the radioactivity of alpha particles travels less distance than the beta particles of the Lu 177.
novartis.com/news/media-rel...
I found this on the internet about Pluvicto and I did search the internet page for "bone" and did not find anything. Sorry, you could be right. I believe actinium alpha particle emiter and Xofigo are probably more useful for bone mets but I could be wrong. Can you please discuss this with your MO or do further search on Google?
Using Lutetium PSMA infusions could be even dangerous under certain condition as it could suppress the bone marrow if the Betta particle emiter Lutetium is panetrated into the bone marrow.
If your intention is to cure bone mets be very careful what you are doing and you could maybe join the clinical trial in Sydney in Darlinghurst conducted by professor Emmett.
clinicaltrials.gov/ct2/show...
It is above my pay grade. Sorry
More about Lutetium PSMA therapy for you:
Lu 177 PSMA is as good as other therapies for MCRPC which usually control the cancer for 3 or 4 months longer than SOC .. The same happens with chemo, Xofigo, Provenge etc.
All the cancer therapies do not work well when used in patients with very large tumor load and with multitude of treatments. Unfortunately most of the clinical trials are done in this type of patients.
Why is it so that the liquid biopsy yield with better results when the PSA is above 10 and bone metastatic?
The liquid biopsy works if enough cfDNA/RNA and circulating cells are collected in the blood sample.
It seems is related to the tumor load. There was a study some years ago showing that in people with few bone mets and PSA below 10, blood the samples did not had enough cell free DNA/RNA and or circulating tumor cells to do the genetic and IHC studies.
Do you have the link to that study? I would like to read it. This liquid biopsy is not cheap.
a recent article indicating that a least a PSA of 5 is needed to have a good yield in a liquid biopsy along with higher ALP (bone metastases) and other variables.
The highest the PSA and the tumor load determine by the present of bone metastases, the chances that a good yield of tumor DNA will be obtained in the liquid biopsy.
I had lot of bone mets. Professor Richard Epstein said to me at the very beginning that some people live long with ADT alone. I think 7% live longer than 10 years.
Is both a PSMA scan and a FDG scan needed to check heterogeneity of Prostate Cancer for LU-177 (Pluvicto) treatment in the US?
No, it is not needed.
The Hofman’s group in Australia started to use it in a randomized control trial to select patients who will benefit more from Lu 177 PSMA treatment. For example, if a FDG PET/CT showed tumors which were PSMA negative those tumors will not be treated by Lu 177 PSMA treatments and those patients were not admitted to the trial.
Other criteria to select patients had been used in trials such as mets with SUV values similar to the liver or at least one met with a SUV of 20 or more. These criteria eliminated all patients which did not have metastases with those values.
More recent they are concentrating the selection of patients using the whole body mean SUV value (do no ask me how they can calculate this value) and based in this value decide which patients will benefit from Lu 177 PSMA treatment.
If one has a cancer with low PSMA expression (mets SUVs less than the liver) , a FDG PET/CT may be useful to make a final decision about treatment with Lu 177 PSMA, since there may be mets which are not seen in the PSMA PET/CT and appear in the FDG PET CT.
Other criterium which could eliminate patients for Lu 177 PSMA treatment is diffuse bone marrow infiltration in a PSMA PET/CT.
If these patients are treated with Lu 177 PSMA, many normal blood cells in the bone marrow could be affected by the radioactivity of the Lu 177 PSMA attached to cancer cells in the proximity and make the hematological problems even worse.
The bone marrow of these patients could be affected less if they are treated with Ac 225 PSMA since the radioactivity of alpha particles travels less distance than the beta particles of the Lu 177.
This was a comprehensive and to the point explanation., May I add; Enza treatment usually doubles the PSMA density. luPSMA treatment in India is 5500 USD, they also have a combo low dose ac and normal dose lu. But, you have to find out about the PSMA density and if you have negative PSMA lesions.
Honestly this Lutetium PSMA therapy is a nightmare scenario for me.
I am waiting for the j591 version of the Lutetium and Actinium.
You have it as a clinical trial in the USA now.
I understand you perfectly well. Worst scenario is having lesions with low SUV and other lesions that is PSMA negative, if you then use acPSMA you end up accelerating the cancer growth and introduce Xerostomia. Best scenario is high, consistent SUV uptake, no liver mets, BRCA2 mutation, you can achieve a result where the PSA drops to undetectable levels.
Which scans did you use in order to find a visible bone mets?
If the bone mets were only detected on the PSMA PET scan than Nubequa (Darolutamide) would have a least side effects on you, and it is approved for CRPC with no visible mets on the bone scan/CT. Therefore insurance would approve Nubequa if you only have visible bone mets on PSMA PET scan an not visible on nuclear medicine bone scan plus CT.
I've had two PSMA scans in the last two years. Both detected three small bone mets. Three years ago though I had an Aux scan that found cancer in my seminal vesicles. That was treated with Proton.
You are doing fine just try to convince your MO that you need Provange. SBRT plus immunotherapy is a winning combination for you rather than a life changing Lutetium infusions which could damage your kidneys and result in repopulation with PSMA negative cancer and render unusable for the future PSMA PET scans.
Your MO could use CEA test to see how your treatment is going.:
google.com.au/m?q=CEA+blood...
You are eligible for Nubeqa if only the PSMA PET scan can detect your mets.
You really want a competent MO to make decisions for you and not a forum like this.
Of course you should have control and feel comfortable what they are doing with you and don't go down the experimental rabbit hole.
Just don't jump early into Pluvicto or Actinium just because someone bullied you into that at PSA 0.3. wright?
I personally believe (my hypothesis) that Provange is maybe effective against prostate cancer stem cells.
That could be the reason that it extends life without reducing the PSA.
Ask your MO about a possibility of chemotherapy before or parallel to Nubequa.
I believe ones you start Abiraterone plus Prednisone you lose the chemo option early. Again I don't really know this as maybe chemotherapy is not recommended for you for your early stage. Still ask your MO about that combination.
One more thing to consider is that 15% of people on Enzalutamide develop a neuroendocrine version of the cancer and that is really bad for you.
That is one of the reasons that untill now I am only on Firmagon (ADT) injections and had early docytaxel chemotherapy.
I just recently (on Monday) finished SBRT-ing my prostate and despite all what I said to you I don't have a guts to start Enzalutamide.
My PSA dropped from 1.4 to 1.2 after the 4 th fraction of the SBRT to my prostate. I will see the RO in 3 months.
This SBRT procedure may not extend my life but makes me sleep better without worrying about the neuroendocrine version of the cancer.
I received 38 Gy to my prostate in 5 fractions.
My SUV max value of the prostate gland was 14 on the PSMA PET scan. Therefore a recommendation to SBRT my prostate.
On the PSMA PET scan I didn't have any visible mets four years after starting Degarelix ADT injections.
I also had an FDG PET scan and a bone scan to make sure that my mets are still hormone sensitive.
The cancer in my prostate was CRPC and I had to choose the next move.
Chemotherapy (with all the side effects), Enzalutamide with the possibility of getting the neuroendocrine version of the cancer.
Therefore I made a decision to kick the can down the road and to get rid of the CRPC in my prostate by SBRT ing it.
Hey Seasid
My husband had his first PSMA pet and I couldn’t find any SUV value mentioned in the report No did anybody mention it? It’s pretty new here, only been doing them for a couple months
How do we find out from RO if SBRT would be an option
He’s having a prostate biopsy today for sample tissue sent to Caris labs for testing, his MO wants us to wait the 2-3 weeks before next steps. He’s been on ADT +Zytiga and Pred for about 10 days , very few SE except for the fatigue , thanks in advance
I asked for a referral to the RO from my primary care physician and then the RO sent me to have a PSMA PET scan.
From that scan the RO concluded that I have cancer in 95% of my prostate with the SUV max value of 14.
My MO RO and me agreed that the best course of action for me is to irradiate my prostate.
I don't know your situation.
When I was diagnosed with multiple bone metastasis they advised me against radiation as it would not extend my life according to a Stamped trial.
But now after more than 4 years on ADT my PSA started to rise. Therefore we concluded that the cancer in my prostate is CRPC now and I don't have visible mets. Therefore irradiating my prostate would get rid of the CRPC and allow me to hopefully stay on Degarelix injections alone.
You may want to see an experienced RO and an experienced nuclear medicine department.
I am lucky that I have it in a same area where I live.
This is my personal situation.
You really need good team of doctors.
Is your husband now without on the PSMA PET scan visible mets?
What was his original diagnosis? How many mets did he have?
I am not a doctor. Try to get a second opinion.
While I am certain Tall_Allen's advice is solid.At some point you will want to consider bipolar androgen therapy.
I would start getting some second opinions on that now.
Read of good results on a trial using a prolactin blocking drug for your type of cancer
I remember a member discussing Steady State PCa, or treating to keep the cells in a Senesence setting. Can't find the thread any more. But something worth looking up. We always want to treat to "kill" or try to kill cancer cells... But what if we could just slow it down and out it to sleep, live side by side with it?
I know, and my genomic testing shows, distinct changes (somatic) post salvage RT & ADT. Was it always there? Or was it induced by therapy? For me, we will never know because I chose my path. But is an interesting avenue not discussed often. We want the hammer, when sometimes, doing just enough for a response is well worth it. And what I mean is the conundrum of lines of therapy applied to the cancer. Who's says it's not ok to go back, or step back and use a drug that may be approved in a previous stage, that would work in a later setting. Here, discussing Darolutamide in a metastatic setting!? Arrrrgh... The horror of thinking outside the box! Is using Abiraterone after *lutamides not ok? Why does that type of drug (Abi) get lined up as a predecessor to others...? We know how drugs get approved in late stage therapies first and are slowly walked back by the FDA, why? Once a drug has shown efficacy to the cancer itself, who determines what "stage" for it to be used? Would Keytruda work as first line therapy? Hmmmmm... Why the artificial hurdle be put in place for "progression" on other drugs, or metastatic disease being evident? It's a problem for the patient.
Maybe if those reviewing and approving these drugs and their use actually were patients, things would change!
Just bouncing arbitrary thoughts at this thread.
Best Regards!
I did in fact have aDNA test done at City of Hope last summer and the result: NEGATIVE whatever that means.
About this test
This diagnostic test evaluates 155 gene(s) for variants (genetic changes) that are associated with genetic disorders. Diagnostic genetic testing, when combined with family history and other medical results, may provide information to clarify individual risk, support a clinical diagnosis, and assist with the development of a personalized treatment and management strategy.
You are getting a lot of varying personal viewpoints here, SViking. So I will try to keep my suggestions brief.
1) Yes, get the PSMA PET scan as you have scheduled to see where cancer remains. If oligometastatic, (few sites) then pursue SBRT to target them with IMRT. If in pelvis add SRT to the full pelvic lymph node beds.
2) Since you are now metastatic and CR you are eligible for Provenge paid by Medicare. Get it! No need to wait. It is an independent line of beneficial treatment with very low risks. Works even better in conjunction with the SBRT.
3) You need to add an advanced androgen targeting drug to your ADT. Zytiga with the low dose prednisone is actually a very good choice and is quite inexpensive as generic at 250mg with breakfast dosing.
I think Nubeqa has several advantages over Xtandi, especially with side effects and possibly with less mutation induced resistance pathways. But you will need to have a plausible reason for your MO to apply for authorization. For me, I “may” have had seizure activity from an unrelated drug in the past. So I would justify I need Nubeqa for the reduced seizure risk. If one tried Xtandi first and had severe disabling fatigue (it happens), then that could also justify Nubeqa as it does not cross the blood-brain barrier.
4) If the PSMA scan shows even moderate avidity (SUVmax) at metastatic sites, then I would pursue Pluvicto Lu177 treatments. Yes, lymph node disease may respond better more often than bone met sites. But it is not fully predictable, the majority (2/3) obtain some clinical benefit even if not among the best responding (1/3). Perhaps the Xgeva has helped protect your bones from many mets.
Don’t panic Viking. You still have weapons and arrows in your quiver. Paul
I agree with you. Looks we are getting the same information.
I am myself considering Lutetium and or Actinium but only hopefully for a very distant future. It is good to be informed as much as possible but I really would not rush myself.
The concern is in a long term side effects from radiation. We have to be realistic that this PSMA technology is only in it's infancy and very soon we will know much more.
If you don't need to rush it is better to wait until more data is available in USA.
If you want early intervention with Lutetium or Actinium better if you go to Germany, university hospital in Heidelberg.
This is only my opinion and you are welcome to discuss this with your oncologist. I am getting all my information from this site therefore your oncologist may know more than me.
thank you so much. I will bring this up with my oncologist when we get the new PSMA report.
Given the extensive commentary on Pluvicto here, please check out this info, which is probably the most comprehensive explanation to date.
What is SVs?