When to start salvage radiation therapy
Just a quick question.
I have found different psa values recommended to start salvage radiation therapy.Apparently to my understanding the earlier the better.
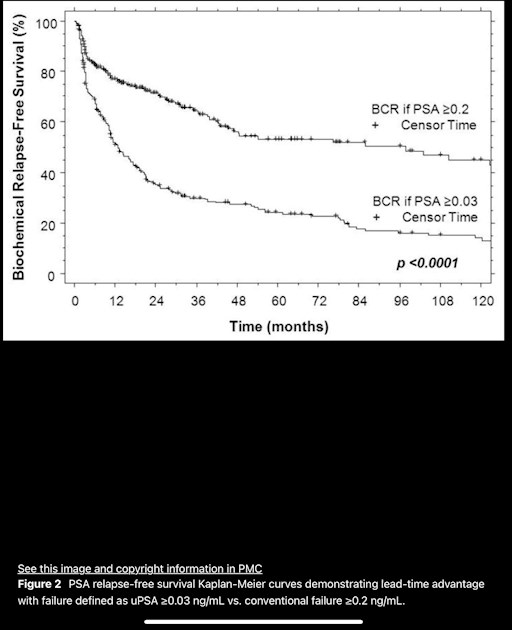
I found different numbers ranging from 0,03 to 0.2 with a huge difference in relapse free survival