Hi there, I was diagnosed hypothyroid 6 months ago and am being treated with thyroxine (now 150mcg). Wasn’t feeling better so after reading posts on this page asked my gp for more blood tests (as early as possible and fasting with no thyroxine). Am looking for help interpreting the results and for any suggestions as to what might help me feel better. Thank you in advance.
Help with blood results: Hi there, I was... - Thyroid UK
Help with blood results
Thank you very much...there are so many variables that it’s pretty confusing. Hopefully my gp will allow me to increase thyroxine dose though she already thinks 150mcg is high. Based on those numbers are there any supplements you’d recommend?
It is high if you are overmedicated and it is low if you are undermedicated. You are undermedicated and need a higher dose of thyroxine. It is hardly rocket science what is wrong with these doctors 🙄they are afraid of their own shadow! Good luck with educating her and getting the increase you need ☘️🍀☘️
Thank you for your reply...yeah, seems to be an up hill struggle. Need to find a dr that has underactive thyroid!
I did find one by pure chance not design and she was really awful! Cutting my medication by half in one fail swoop after I’d had 9 months of hell getting it to an optimal level under the care of an endocrinologist. I thought no way are you putting me back to the pitiful state I was in on that minuscule dose! It was nowhere even near a full replacement dose and I had no thyroid function whatsoever. It was an idiotic thing to try and do. I was on to the endo sec immediately she told me to tell the doctor to refer me back to them for further assessment before any dose alteration was to be made. She dropped it like a hot brick claiming she did not have the hospital reports or the results - fantastical she had my medical file and they were all in that! She had not bothered to read them would be more accurate. She looked really unwell thinking back. Despite her having the condition, I found GP’s who were far superior in treating it but were not hypothyroid themselves! You’d think having it yourself would accord you empathy and expertise in treating it in others if you were a GP. I was a bit shocked to discover one does not necessarily lead to the other! I switched GPs fast!
You just need a competent GP who listens, is knowledgable about the condition, how to treat it and optimise that treatment and is up to date on the latest research and developments. A rare breed but some do exist! If you are in the uk, Thyroid UK admin have a list of sympathetic medics you can ask for but I am not sure if it is just of private doctors and endos. You could tell them where you are and ask if they could point you towards anyone who has been recommended to them.
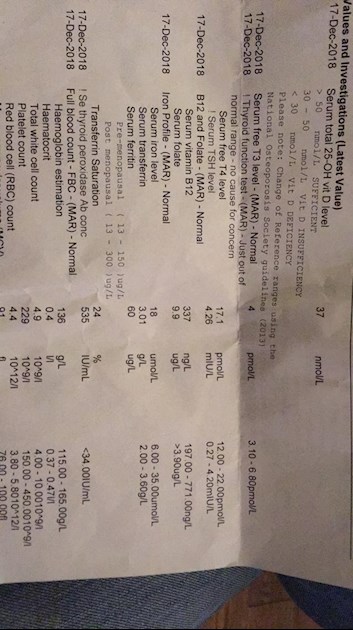
Vit D 37 mnol/L no range
B12 337 (197 - 771)
folate 9.9 >3.9
ferritin 60 (13-150) pre-menopausal
(13-300) post-menopausal)
They all look a bit low to me.
Read up many of SeasideSusie excellent detailed replies to others on low vitamins
Did you know you had Hashimoto's?
Your antibodies are high this is Hashimoto's, (also known by medics here in UK more commonly as autoimmune thyroid disease).
About 90% of all primary hypothyroidism in Uk is due to Hashimoto's
Hashimoto's affects the gut and leads to low stomach acid and then low vitamin levels
Low vitamin levels affect Thyroid hormone working
Your are all too low
Poor gut function can lead leaky gut (literally holes in gut wall) this can cause food intolerances. Most common by far is gluten.
According to Izabella Wentz the Thyroid Pharmacist
approx 5% with Hashimoto's are coeliac, but over 80% find gluten free diet helps, sometimes significantly.
Either due to direct gluten intolerance (no test available) or due to leaky gut and gluten causing molecular mimicry (see Amy Myers link)
Changing to a strictly gluten free diet may help reduce symptoms, help gut heal and slowly lower TPO antibodies
Ideally ask GP for coeliac blood test first Or buy one online for under £20
amymyersmd.com/2017/02/3-im...
chriskresser.com/the-gluten...
thyroidpharmacist.com/artic...
scdlifestyle.com/2014/08/th...
drknews.com/changing-your-d...
That’s brilliant advice...thank you. I’m reading the Thyroid Pharmacist but there’s a lot of information as well as all the different units etc. I’m going to have a look at the SeasideSusie replies now. I’m so glad I found this forum...I feel more confident about pestering my gp now. I’m so used to feeling rubbish that I’d become a bit resigned to it.
Getting vitamins optimal can make significant improvements and is first steps. It often improves conversion of FT4 to FT3
Plus 25mcg dose increase in Levothyroxine. Aim is to bring TSH down to around one and FT4 towards top of range and FT3 at least half way in range.
Retesting thyroid levels 6-8 weeks after dose increase
All thyroid blood tests should ideally be done as early as possible in morning and fasting. Do not take Levothyroxine dose in the 24 hours prior to test, delay and take immediately after blood draw. This gives highest TSH, lowest FT4 and most consistent results. (Patient to patient tip, best not mentioned to GP or phlebotomist)
Then in New Year consider trying strictly gluten free diet for 3-6 months. If it helps stick with it. If no apparent benefit, retesting antibodies before starting back on Gluten (antibodies often drop when GFree). Reintroduce gluten and see if symptoms get worse
Dr Toft, past president of the British Thyroid Association and leading endocrinologist, states in Pulse Magazine,
"The appropriate dose of levothyroxine is that which restores euthyroidism and serum TSH to the lower part of the reference range - 0.2-0.5mU/l.
In this case, free thyroxine is likely to be in the upper part of its reference range or even slightly elevated – 18-22pmol/l.
Most patients will feel well in that circumstance. But some need a higher dose of levothyroxine to suppress serum TSH and then the serum-free T4 concentration will be elevated at around 24-28pmol/l.
This 'exogenous subclinical hyperthyroidism' is not dangerous as long as serum T3 is unequivocally normal – that is, serum total around T3 1.7nmol/l (reference range 1.0-2.2nmol/l)."
You can obtain a copy of the articles from Thyroid UK email print it and highlight question 6 to show your doctor please email Dionne at
tukadmin@thyroiduk.org
New NHS England Liothyronine guidelines November 2018 clearly state on pages 8 & 12 that TSH should be under 1.5 when on just Levothyroxine to be adequately treated
sps.nhs.uk/wp-content/uploa...
Professor Toft recent article saying, T3 may be necessary for many or we need high FT4 and suppressed TSH in order to have high enough FT3
Thank you...Another trip to gp after Christmas then. I’m also going to try gluten free now that I know it’s Hashimotos.