O.Mowforth
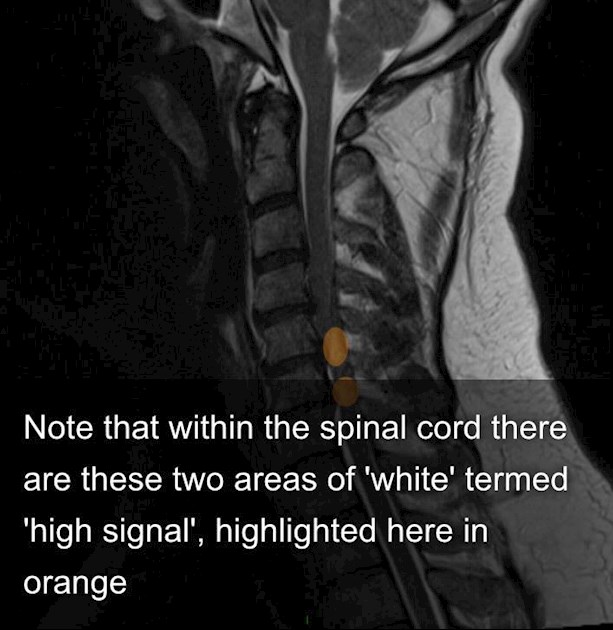
Note that within the spinal cord there are these two areas of 'white' termed 'high signal', highlighted here in orange
Images courtesy of Radiopaedia.org
MRI imaging is the mainstay of diagnosis of patients with CSM. Whilst the MRI can described findings associated with myelopathy, there has been a lot of debate as to whether it can tell you how bad your myelopathy is, and whether or not you would respond to surgery.
In this regard, changes within the spinal cord itself have been a major focus. MRI images are black and white. When you undergo a MRI scan there are two principal image types that are produced 'T1' and 'T2' images. The sequences highlight different features, and therefore what is white will differ from one sequence to the next.
Amongst patients with CSM, most have a 'normal' looking spinal cord, but others can have changes, including high signal (aka the 'white spot') on T2 images, with or without low signal (black) on T1 images.
A group from North America (1), in the largest such study to date, having been looking specifically at changes within the spinal cord. Their theory was that the amount of spinal cord damage, and therefore the severity of disease and likelihood of improving after surgery, related to this sequence of changes. I.e. Normal cord was better than a white spot, but a white spot with corresponding blackness on T1 was worst of all. The white spot is thought to represent oedema, whereas the blackness loss of spinal cord tissue.
The authors analysed over 400 MRI scans of patients who went on to have surgery for CSM. Just as they thought, they found that these image changes did relate to the severity of myelopathy, and likelihood of responding to surgery.
More specifically, they found that the 'black' low signal on T1 images was the most important feature; most likely to be found in more severely affected patients, who responded less well to surgery. A 'white spot' on its own was only very slightly worse than normal looking cord, however 'white spots' at multiple levels was associated with more severe myelopathy.
This is a high-quality study, involving a large number of patients from across the globe. This is a very interesting study and moves the field forwards. The clinical relevance of a 'white spot' was uncertain, and a topic of constant debate; some studies had shown it was a sign of bad myelopathy, where as others that it was not indicative of severity (2). The finding here of the significance of one vs many white spots may explain these previously inconsistent findings. Regardless the relative, greater importance of low signal (black) on T1 images is new.
These image findings are not the be all and end all; some patients with spinal cord changes on their MRI do very well with surgery and vice versa. These findings therefore, at least for now, are only a guide.
References
1. A.Nouri et al. The Relationship Between MRI Signal Intensity Changes, Clinical Presentation, and Surgical Outcome in Degenerative Cervical Myelopathy: Analysis of a Global Cohort. Spine. May 2017.
2. L.Tetreault et al. A Systematic Review of MRI Characteristics that Affect Treatment Decision-Making and Predict Clinical Outcome in Patients with Cervical Spondylotic Myelopathy. Spine August 2013