COVID-19 Vaccine is Safe but 25% Of Blood Cancer Patients Do Not Produce Detectable Antibodies.
More from LLS colleagues here:
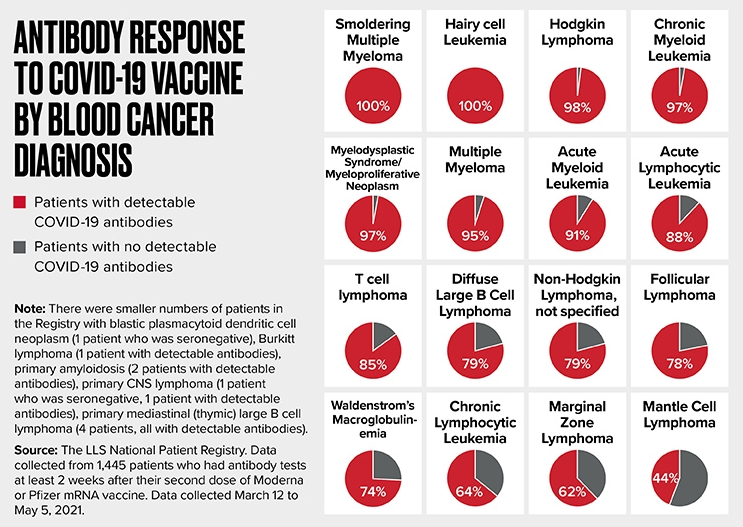
COVID-19 Vaccine is Safe but 25% Of Blood Cancer Patients Do Not Produce Detectable Antibodies.
More from LLS colleagues here:
Interesting. I didn't expect to see so much variation between different blood cancers. Surprising that Multiple Myeloma responds so well to vaccinations.
It doesn't look so good for CLL patients, but if 64% have detectable Covid antibodies after vaccination, that's not too bad. I thought it might be worse.
However, CLL patients may not be doing as well as this diagram suggests, as patients were just tested for detectable antibodies, and not whether their antibody levels were high enough to be effective.
It's still unclear as to what levels of antibodies ARE effective though. Other factors are involved and not just numbers of antibodies. Anyway, any protection is better than none.
Paula
and this
When I see these sort of numbers, I wonder when I will ever be able to get out of "Covid Jail".
Probably when your treatment stops and your immune system has a year to recover? I’m not looking forward to round two of treatment as it will also place me in “Covid Jail”.
Indolent -
My plan is to continue to mask, and keep an eye on local hospitalization and death counts. Case counts are no longer reliable, because testing is no longer mandatory. I stay out of bars and restaurants. I really miss live music. I live in New Orleans.
So, I'm not exactly in jail, I'm out on bail. ;^)
=seymour=
I showed positive for antibodies 14 days after vaccination but lost my antibodies within 1 month, enough loss to register as negative for antibodies at day 30. I think the 2 weeks post vaccine measurement is not a realistic indicator for some of us with CLL. And I am untreated W & W.
Interesting comparison with the other blood cancers.
"Positive for antibodies" is a terrible stretch. Anything above 30 BAU/ml is a positive result, but for a 90% chance of protection from getting sick, you need at least 2000 BAU/ml.
lexie -
I agree that timing of the antibody test is critical - too soon, and plasma B-cells may not have ramped up enough. Too late, and the antibodies made by the plasma B-cells may have waned a bit. But those cells may ramp up faster on the next exposure. So, first vaccine or first infection takes more time to develop antibodies. Booster or reinfection ramps quicker, if not too much time has passed. And that's all in otherwise normal people. Immunologists are rewriting textbooks because of the focus on such things.
For us, there's also some variation in how CLL affects B-cell and T-cell activation and development.
Elsewhere in this thread I asked Yalokin what determines how long an antibody lives. I'm sure it differs from person to person, and is at least somewhat dependent on inherited genetics.
=seymour=
I think they are unrelated.
w and w, but hit 30 ALC mark this year, and put onto yearly tests.
4 of my 5 vaccines I've had a reaction to, usually 2 weeks before driving again.
Got tested through monitor my health 6 weeks after 5th vaccine, early July, got more than/ equal to 2,500.
Gonna test again in a month from now to see what I retain.
MickDerry -
Good idea! Time is a factor.
I had Evusheld, and got COVID. A month after COVID, I had >3000 U/mL on the LabCorp (Roche) spike IgG test. Do I feel "protected"? Surely not. I do feel somewhat armored, and probably won't die. I also wonder how long the armor it will last, and whether some future variant can penetrate more easily.
Anyone who had their last vaccine or Evusheld dose 6 months ago, probably has very little biological armor left.
Well-fitted N95, KN95, or KF94 Masks are proving to be pretty good armor to add to the biological armor.
=seymour=
3000x0.97 =2910 BAU/ml- very good levels.
Ah, yes, good levels. But good enough? And for how long? Evusheld was not good enough to prevent a symptomatic infection with fever for me, despite Paxlovid. I was 85U/mL after the 4th vaccine shot (a half dose of Moderna). I am W&W.
The lifetime of antibodies - even long lasting ones - is a bit of a mystery. Just what determines the lifetime? I know they modified the fc stem of these antibodies to make them last longer, but how does that work, exactly?
=seymour=
Eye protection too. Moisturizing eye drops if clear goggles or glasses are a problem. Eye exposure is a really really small risk, but it's there and if one has to be in crowded rooms, on public transportation, or outside on windy days, I think it's worth the bother. I am convinced I caught a cold from workmen across the street; I could smell their cigarette smoke and it was windy. Some of them were coughing, and a few days later I became ill. I was Covid negative, but with the problems with testing and the "windows of positivity" who knows. Since I hadn't been to the grocery or other public place, not even a park, this is the only exposure I can recall having.
Does CLL stage makes a significant difference here? I am Stage 0 and W&W (for 4 years now) and mounted significant antibodies. Just curious why some of us seem to do well with the vaccine while others do not. <3
I wouldn't think so. IMO the ability to make proteins, specifically antibodies, is the issue. Whether our CLL is affecting our number of enlarged nodes, or ability to make platelets, or if we have an enlarged spleen, probably doesn't affect antibody production to a great extent. Someone could be in the earliest stage of either Rai or Binet staging, and struggle making serum proteins like albumin and antibodies. I would think that there might be a correlation; those with low level disease are probably more likely to have near normal body functions. But not causation; later stages of the disease may not necessarily correlate, since "levels of/ability to make serum proteins" isn't used in staging.
how many are your antibodies, if it's not a secret?
Here's my results (attached). This is after an initial 2 Moderna shots (in Spring of 2021) and then a Moderna Booster in September of 2021. Then a final 4th shot (Pfizer) in January 2022. These results were from March 2022. I don't have anything more current. I have not had anymore shots other than these 4.
I did finally contract Covid for the first time in July 2022. I had a mild case, took Paxlovid on the first day of symptoms. Got better two days later and tested negative by day 5. Sadly, I got the dreaded Paxlovid Covid rebound less than a week later and got much sicker with the second round. However, it was still considered "mild" and isolated to upper respiratory. Nothing in my lungs and no fever or cough to speak of. Just a lot of sinus pain and pressure and a general feeling of being unwell and extra tired.
Whenever there are percentages, there's more to the story for individuals. One should not make decisions based on percentages from a group of patients without asking if there's a way to measure yourself against the others. Sometimes there is, and sometimes not. In this case, one can do the antibody test before and after a shot to see.
I think the 64% is an aggregate of all the patients in any treatment class who made any antibodies at all.
I think it's sad that LLS defined the response as "detectable antibodies." Some doctors have used that definition to deny access to Evusheld, Paxlovid, Bebtelovimab, etc. It would be better to say that 36% made no antibodies at all, I think. That emphasizes the vulnerability rather than the (mistaken) apparent success.
It's also certainly possible, but not probable, to not be in treatment at all, and not have a vaccine response at all.
As others have said, antibodies are a simplistic way of looking at immunity. Dr. Thompson at M.D. Anderson reminded me that CLL patients usually also have a restricted T-cell response - you could have a lot of T-cells, but they might not bind your favorite antigen very strongly.
=seymour=
Jammin_Me -
And habitual shorthand by both scientists and journalists doesn't help, either.
=seymour=
Thanks for posting Yalokin, especially the graphics.
As COVID-19's evolutionary tendencies seem to be transmissibility and immune escape, I wonder if the notion of a number as a correlate of protection is just not meaningful.
When we measure our antibody levels after vaccinations and/ or Evusheld and/ or past infection, we should ponder: antibodies against what? how would these antibodies do at neutralising a future infection? After all, many healthy, fully vaccinated individuals have had COVID in two/ three flavours.
Moderna's Spikevax and its competitors should take the immunocompetent population back to square one - but only for a while, until new evasive variants emerge. In that case it's important to realise that although the virus might not cause severe symptoms in most, it would remain in circulation.
In CLL many of us don't do antibodies anyway. The ideal correlate of protection would be some measure of the state of readiness of the individual's cellular response to a future COVID infection. Ideal but too hard to measure. Perhaps we can use antibody levels as a surrogate marker? At one point in the Birmingham Uni study that seemed a possibility. We need to see their study report in detail, and the few other studies out there. Updates anyone?
NB here I'm suggesting antibody levels as a correlate of protection, not against catching COVID-19 but against getting seriously ill.
See here: degruyter.com/document/doi/...
Thanks. I think I see where you're pointing with this, but it's in a different direction to where I'm going.
If I understand it right, the paper purports to establish a threshold antibody level, for a particular serology test and a particular vaccine, corresponding to a level of neutralising antibodies measured by a different test. Ergo, correlate of protection.
Fine. Except that it was all done in a 3 month period ending in February 2021, when Italy would have been in the grip of the Wuhan and Alpha strains, both highly susceptible to neutralisation by vaccine. Delta and Omicron had not yet emerged. Actually neutralising antibody level was first "established" as a correlate of protection against COVID in August 2020.
Talking about binding and neutralising antibody levels still confines us to the humoral immune response, which, even in the immune competent, decays over months and can be sidestepped by emerging viral variants. What we, especially we immunocompromised, need is a surrogate marker for cellular immune response, which is comparatively broader and more durable.
I agree. It's just a guideline. In my opinion, nothing is completely clear about the immunity issue. The virus is constantly mutating. This morning I read about a forecast for an even more aggressive virus. Where will this madness end and at the cost of how many human lives? Me personally I lost several very close people. At 53-60, 62 years old.