Hi thank you for allowing me to join the group and was wondering if this is still active but I’ll post my query here.
white female, 39 years old (38 at time of spirometer) 166cm tall, weight 55.0kg
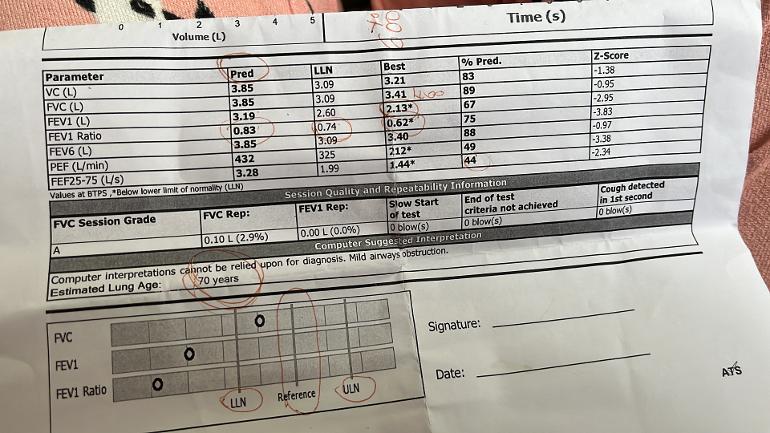
November 2023 I come down with that horrid virus that’s fleeted us and was generally unwell with it, and come December I started really experiencing a tight chest and breathlessness on exertion. I forgot to mention that I got taken to a&e Christmas Eve due to feeling very poorly with chronic headaches, vertigo, and generally unwell, and had a ecg done was tachycardic but that’s normal for me when unwell, bloods done showed slight infection, and had a xray that was also clear, and was told go to your gp when it reopens so went to the gp who said my breathing issues of breathlessness and tightness was anxiety induced trialled ssris that made my breathing worse, so got put forward for a spirometer test, I failed at a reading of 63% to the 74% needed and shows signs of obstruction , I didn’t have the reversibility test done as nurse said if I didn’t think I had asthma then no need and quickly said straight away copd try this inhaler, ended up in a&e as the inhaler was causing to me at the time burning sensation and stomach aches, put it down to the inhaler stopped it tried anora ellipta again no difference and made me feel worse, so trialled the clenil modulite 100 inhaler that didn’t work and made me more aware of my burning and menthol sensation that I have had since January, so now I’ve stopped the clenil inhaler as I went to hospital with tachycardia and repeated ecg, bloods, and second xray that also come back clear with no scarring, no infection, and no sign of copd scarring, not to say I haven’t got it as I still could they said , and noticed for the last 10 days that I’ve had really bad reflux and gp said that the reflux could be contributing to the breathlessness and tightness and to take lansoprazole which I have been religiously and now my breathing seems to be improving slowly each day, wondering if this is the reason to my breathlessness and tightness and read that you can get adult induced asthma from reflux, does these symptoms coincide with this? Or am I being wishful thinking? I’m not denying I have lung issues as I failed my spirometer.
My only symptoms are breathlessness on exertion at times, tightness of the chest, odd pain now and then now I’m on lansoprazole and that’s it and obviouslymy reflux symptoms of hoarseness of the throat at times, sore gullet, stomach aches, burning and menthol feeling both In chest and throat and when eating, burps.
Sorry it’s so long but I wanted to get as much I. The post as possible, and thank you if you have managed to get this far and I appreciate it a lot xx