Four years ago (2009) I had an operation for cancer (confirmed) and in 2011 I had another operation for for a suspect nodule (nothing nasty found this time).
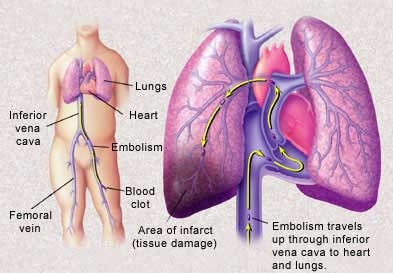
In the last four years I have lost count of the number of DVTs and PEs I have had. I have had three hospital admissions (the last one, in August, for three weeks) and I don't want another one. The 'run up' to the hospital admissions is most distressing - I can cope with the aches and pains but not the feeling of being unable to breathe.
I was originally prescribed Warfar and was on it for quite some time. My last hospital admission showed that the Warfarin had not been working and I was prescribed Dalteparin which I inject daily.
It was suggested, by the doctors, that I have a valve implanted in my vena cava (I think) but that's on hold for the moment.
What I could do with is some suggestions on how to avoid DVT's. Should I avoid eating certain things?
Annec