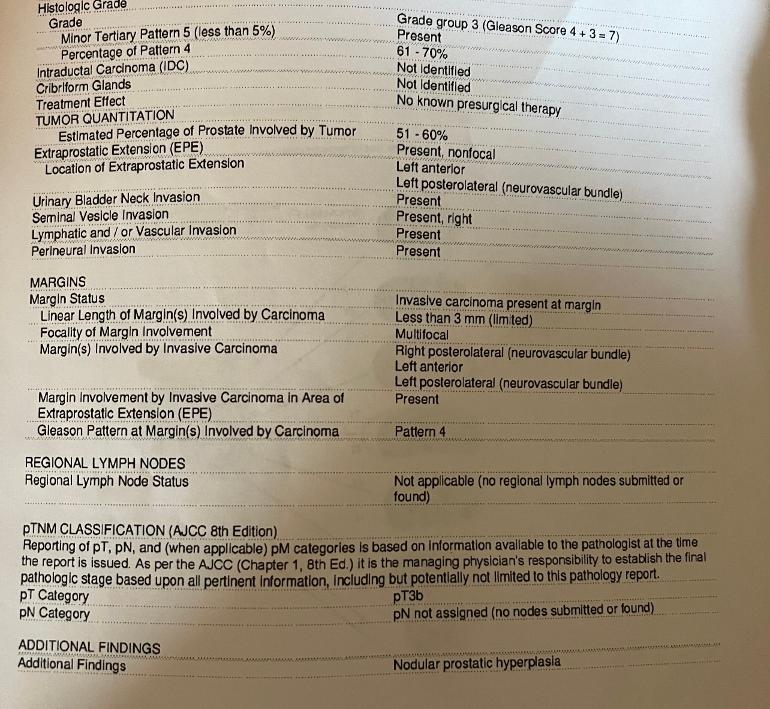
my dad got his pathology report following prostatectomy what does this all mean doesn’t look confirming
pathology report : my dad got his... - Advanced Prostate...
pathology report
(Im not a Dr)
He might be looking at post prostatectomy salvage radiation.
Curious why lymph nodes were not submitted??
The worst finding of all, IMO is the bladder neck invasion. If the surgeon took notice of it during the operation and resected the invaded part this will affect his continence. If not, his BCR free time span may get compromised.
It means that prostatic tumors were large and had escaped the prostate capsule, especially at the seminal vesicles. There are positive margins, which means some bits of cancer were left in his body. And it was pattern 4 at the margin, which means he can't just watch it. Additionally, there was a small amount of pattern 5, which is highly invasive.
I think it's a good idea to:
1) Get a PSMA PET/CT to rule out distant metastases. If clear...
2) Start Lupron immediately to prevent further spread. Hormone therapy will continue for 6 months after radiation begins.
3) When tissues have adequately healed and he is hopefully no longer incontinent, he can begin whole pelvic adjuvant radiation.
I don't think he should wait for a PSA test.
His doctor didn’t seem concerned but when he showed me I went down a Reddit rabbit hole and this didn’t seem correct. Should we see a different Dr second opinions?
He also had a Pet scan MRI all prior to surgery
Everything was clear to go no metastasis
Then he doesn't need a new scan, and he can go ahead with hormone therapy and adjuvant radiation.
Yes, get a second opinion. His is an exception to the general rule that it's OK to wait for a detectable PSAs:
prostatecancer.news/2021/10...
If his doctor is still doubtful that he needs adjuvant radiation, break the stalemate with a Decipher test.
I could not get much traction asking for ART with my "adverse pathology" which in my case was Gleason 9 + T3 (SVI) but zero margins and post-op zero PSA for a year now. Radiology and urologist said they did not think one should treat an invisible condition after RP, even though your article shows ART seems to have a huge advantage in all cause mortality (5% vs 20%+), over reactive salvage? Decipher is not easily available here (Australia).
Is it unusual for a pathologist to read a bx as G 3+4 when even a small amount of G5 is present?
The rule for prostate biopsy is that the second number is the highest pattern present, even if <5%. So, for example, 60% pattern 3+ 35% pattern4+ 5% pattern 5 is called GS3+5 (which is Grade Group 4).
BTW, the rule for whole mount is different. The above would be called GS3+4 with tertiary pattern 5.
I'm really glad that Tall_Allen answered your questions. He really knows his stuff. I had RP almost six years ago and my pathology report was real good. Your Dad has several adverse features in his report including the positive margins with gleason 4. A PSMA scan would be beneficcial, followed by Lupron right away. He can have his radiation after things heal well from the surgery. It is very treatable but I think he wants to get right on it.
My report was very similar to your dad’s , 5 years ago. Back then PET scans were not widely available, I barely had heard of them and it wasn’t mentioned anyway. The only real difference was I had negative margins, but the other adverse features were there.
Fortunately the surgeon decided to not advise me to just cruise on. That yours ‘didn’t seem concerned’ is unsurprising. This is precisely what so many urologists do even today with this type of post RP pathology. Instead I was referred to a MO at the same institution . He recommended a clinical trial. The additional treatment was basically what’s been described to you in the comments here.
It was challenging at points but not overly so. As of today i am doing well, no evidence of disease and on no drugs.
My suggestion is to get him on the path that you’ve been recommended here now, regardless of what the urologist says. Acting swiftly may easily make the difference. Great luck to you!
That biopsy report was so readable and short that I saved it for comparison to mine. My 2021 biopsy was 17 pages that looked like they were cranked out of a 1980's printer.
First order of business: Find a medical oncologist to advise and guide your father for his future. The best you can find and afford, especially if it is a prostate experienced M. O., regardless of distance within your budget of cost and time.
The surgeon-urologist will continue to follow your father for his recovery and any associated urologic issues such as healing, continence and so on. The next step of his life depends on the best advice and guidance from someone who is experienced with cases such as his. It took me 18 months after my surgery to discover this path. It has served me well.
I noticed several people talking about prostatectomy. My oncologist said it was useless if there was spread to the margins. His Gleason numbers are the same as mine, but I did not have the bladder and lymph metastasis . I would definitely speak with a Medical and radiation oncologist before doing anything else. More likely a candidate for HDR brachytherapy and radiation with hormone suppression treatment.
Well that what’s the whole point of his PET SCAN to make sure it was within the prostate capsule and he was good for a prostateectomy and everything checked out fine this is why am having a hard time understanding all this. His Dr did all the precautionary testing before proceeding with the surgery he did mention is there was a spread it was not worth taking out prostate.
Please update your dear Dad's bio.... It's voluntary but helps him and helps us too. Thank you!
Good Luck, Good Health and Good Humor.
j-o-h-n
The Decipher test is covered under Medicare specifically for patients with localized or regional prostate cancer who are being considered for treatment. This includes those at diagnosis and post-surgery patients with varying levels of prostate-specific antigen (PSA) (DecipherBio). Medicare covers the test, acknowledging its value in providing insights into the biology of the tumor which can help guide treatment decisions (DecipherBio).
The Decipher test does not require an additional procedure if tumor tissue is readily available from the patient's prostate surgery, making it accessible under Medicare coverage without extra procedural requirements. Read everything Tall Allen writes. Don't wait on the prostate bed radiation long.