Click link for animated video:
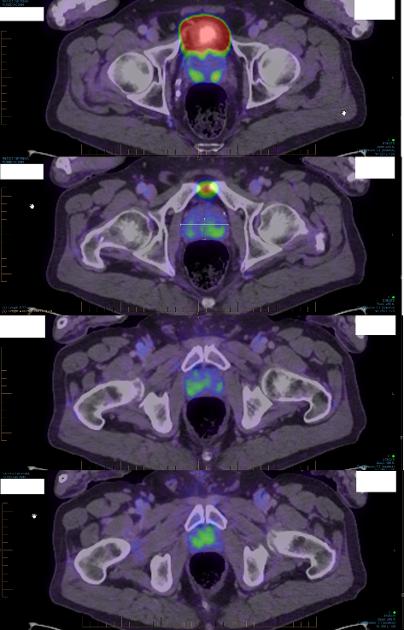
My recent PSMA is shown with 4 images in order. Right-click image, open in new tab to zoom in. What do you see? Does this look bad news to you or of serious concern? Would you suggest RP, radiation, or AS?
My urologist seems to have taken this PSMA scan to supersede all my previous tests as the reason to suggest I have RP (as he said: "if it was me...") and that I see his urologist colleague who does robotic RP (as he is older and does not know that technique, only open RP). Uro2 staged me as pT2c (why the "p"?? error?) but seems based on biopsy/MRI/PSMA not DRE. Anterior TZ tumors are not even palpable, right?
First uro was uncommunicative, pushy and only recommended his TP biopsy. Did not even do DRE. I changed uros.
Second uro: did his suggested TP biopsy. He did DRE but didn't say what he felt. I have asked him to report that result.
Scans seem to be increasingly recognised and PSMA even more so for clinical considerations prognosis. Many articles seem to be out there considering how staging will in future be affected by PMSA so the old-fashioned past methods of DRE only may change in future.
Some of you on my recent post here said I am NOT a candidate for RP but for AS and you suggested I am LOW risk. Why? But you have not examined me fingerwise or otherwise so on what basis do you suggest it? More details below.
I certainly do not want the side effects of RP and currently am thinking of a plan to pursue repurposed drugs (Metformin, Atorvastatin, etc) and AS. I will maybe meet uro's colleague for another opinion but I imagine he will simply suggest RP.
PSMA (7/23)
Report:
PET/CT 18F PSMA
237 MBq F-18 PSR. 140 mL Omnipaque 350
Group 1 carcinoma prostate.
Tumour:
Multiple foci of intermediate PSMA avidity tumour within the prostate
gland.
No seminal vesicle involvement.
Nodes:
No PSMA avid pelvic or paraaortic lymph nodes.
Metastases:
No PSMA avid skeletal or other metastases.
CONCLUSION:
T2 N0 M0 prostate carcinoma
According to PSMA report, no metastases. Good. But what do these lit up areas mean?
PSA:
Two PSA tests in the last week (8/23) were 6 and 7 (7 when done 2 months ago) so I think 6-7 is my PSA although it changes by at least 0.5 every test (??).
MRI (5/23)
Second MRI done (following MRI 6 months ago (PIRADS3). Now suggesting one PIRADS4 right anterior TZ that has increased on scan from 6 to 12 mm in 6 months, and PIRADS3 left TZ 12mm and stable from 6 months ago. Thus bilateral via scan.
Report:
PI-RADS 4 lesion right anterior transitional zone towards the apex. High risk.
PI-RADS 3 lesion left anterior transitional zone towards the apex. Intermediate risk.
BIOPSY (6/23):
TP biopsy targeted right anterior area with 15% involvement of "combined length of tissue") (8 of 12 cores involvement); nothing in right template (11 cores); and less than 5% of "combined length of tissue" in left template area (2 of 10 cores involvement).
---
Please consider these sample images from PSMA and if you have experience with PSMA, sensitivity, specificity, and all that, what do you think this scan shows? I find "experts" these days are overwhelmed by scans that light up. They make the cover of Nature and Science. For example, with brain imaging, what do they really mean? For the brain vs. mind question, not a lot. With PCa??
How bad does my scan look?
According to uro my risk stratification is: T2c, INTERMEDIATE, FAVOURIBLE RISK.
According to MRI Report, the two lesions are: INTERMEDIATE and HIGH RISK.
Nowhere is "LOW" risk ever mentioned by these "qualified experts".
Thanks for your relevant thoughts.