Hello everyone, Thanks for all the incredibly useful information . Hopkins doctor said my PSMA PET might not be accurate when it reported no mets . I got the bone scan he suggested which also said no mets . The PET report said “ the hyper metabolic mass … involves the left seminal vesicle and likely extends into the left periprostatic tissue.” Members of this site commented that the PSMA PET isn’t the best way to assess cancer in and around the capsule , so the SVI could still be in the capsule . When I asked a Hopkins doctor with experience using PSMA PET in clinical trials about its accuracy he said the PSMA PET was right about 2/3 of the time when it found “ no mets.”
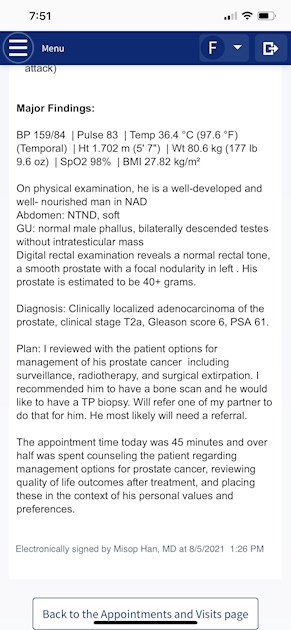
Hopkins doctor reported this after visit on 8/5 : “Clinically localized adenocarcinoma of the prostate , clinical stage T2a, Gleason score 6 , PSA 61. “
He also reported: “Digital rectal examination reveals a normal rectal tone , a smooth prostate with a focal nodularity in left . “
What I don’t get us why Hopkins doctor said I, “may need a referral. “ He’s an expert in da Vinci . He also said RP not possible . He said ,” you’re in bad shape “ and when I asked if he could treat me he said ,” if it’s not too late “ or something to that effect . Not gonna see him again .
I have an appointment at Memorial Sloan Kettering on 9/9 to sort things out with a urological oncologist and a radiation oncologist .
The question is - how bad a shape am I in ? Any comments will be appreciated .
Thanks , Farlow
 monthly and it would be convenient to not have to do that. guess i would still be on aberaterone
monthly and it would be convenient to not have to do that. guess i would still be on aberaterone