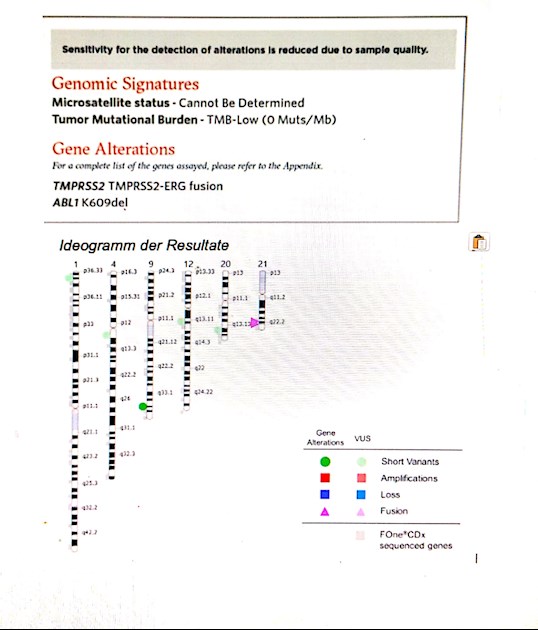
TMB low, Alterations : TMPRSS2-ERG fusion and AL1 K609del
Very low mutation, nothing doable for now from this point. Could it change with time, and if yes, should a new test be done later (must be biopsy or blood test possible?)?
TMPRSS2-ERG fusion: anything to do also in terms of supplements or avoiding foods?
The test was done from one sample, what I don't really understand, since it was not the highest Gleason sample. I mean, they could differ in mutations, no?