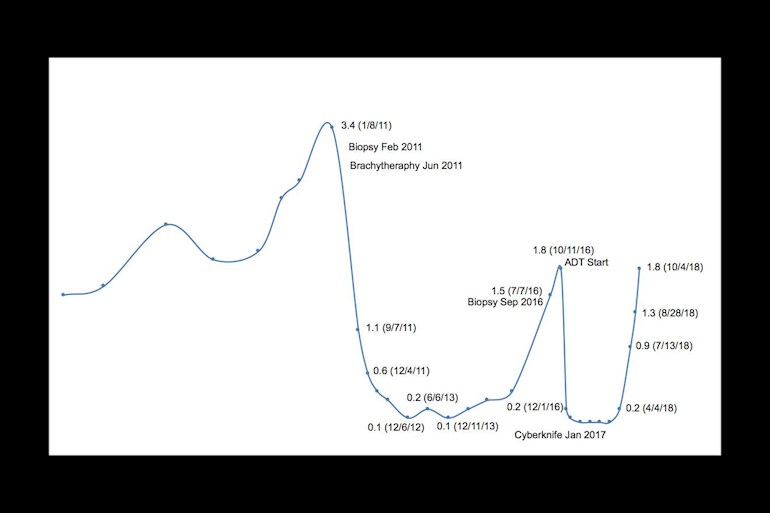
When my brachytherapy for Gleason 6 cancer in 2011 led to recurrence in an extra-prostatic nodule in 2016, I had 9 months ADT and cyberknife. Unfortunately, my PSA started to rise rather rapidly: April 4: 0.2, July 13: 0.9, August 28: 1.3 and October 4: 1.8. PSADT is 2.14 months. The PSA of 1.8 is the same I had in 2016 just before starting ADT. I have an Axumin PT/CT scan scheduled for November 5 at Penn Medicine. By that time my PSA may reach 2.3 or 2.4. My lowest PSA after brachytherapy was 0.1 in 2013. Depending on what the Axumin scan discovers, I may have some treatment options. But I am assuming ADT or intermittent ADT is in my future. My question is when should I start ADT? Should my PSA rise above a certain threshold before starting ADT? Is there any clinical advantage starting ADT soon than later. My PSA history is attached as an image
When should I start ADT treatment? - Advanced Prostate...
When should I start ADT treatment?
Hope you are seeing an oncologist who treats predominantly PCA
He or she can present you options from which you can choose.
Good luck. 👍
This is a recent article about biochemical failure and PSA bounce after brachytherapy.
ncbi.nlm.nih.gov/pmc/articl...
I quote:
"Several guidelines for follow-up after BT for prostate cancer have been described [17, 18]. However, these studies do not mention the factors that distinguish biochemical failure from PSA bounce. When we observe a PSA level of ≥2 ng/ml above the nadir, we check for the presence or absence of recurrence lesions by imaging diagnostic methods, including CT and bone scan. If the increase in PSA levels continues without detectable recurrence lesions, we discuss whether we are observing biochemical failure or PSA bounce, and whether salvage treatment is needed. In this study, the median duration from the date of PSA bounce +2 to the date when the PSA level decreased was 4.5 months, while the maximum duration was 1 year. Sagalovich et al. evaluated the impact of timing of androgen deprivation therapy on survival in a cohort of patients with biochemical failure after BT for prostate cancer [19], but identified no significant difference in survival between immediate and delayed salvage hormonal therapy. The median delay till salvage androgen deprivation therapy in their study was 19 months. We found that a 1-year follow-up after increasing PSA level of ≥2 ng/ml above the nadir with no evidence of proven recurrence did not affect the prognosis of prostate cancer patients. In addition, the time to onset was significantly earlier in PSA bounce +2 than in biochemical failure, as mentioned in other reports mentioned [10–12]. Therefore, 1 year of additional follow-up was useful for distinguishing between biochemical failure and PSA bounce in cases of an increasing PSA level to ≥2 ng/ml above the nadir in patients who were young, had a short time to onset and no evidence of proven recurrence.
"
The results of the Axumin scan will indicate what treatment to follow and when. If there is metastatic disease ADT seems indicated along with Zytiga or chemo (treatments proven to provide a survival benefit in hormone sensitive metastatic prostate cancer). If the metastases are in the lymph nodes only, some may consider radiation or extensive disection. Another possibility could be treatment with Lu 177 PSMA.
MO at MD Anderson said he would start ADT at 1.0 and continue for some period. I don’t know how low but he liked to give body a holiday to reduce long term issues of heart disease, bone loss , diabetes, etc.
That’s a decision that should lie in the hands of a Medical Oncologist who specializes in Advanced Prostate Cancer. We are all different with scope of disease. I have an opinion based on my seeds with 25 sessions of IMRT back in 2003. My PSA never really came down and within 10 or so months, PSA rose dramatically to 32.4 with mets to L2 & T3. I immediately has a Lupron injection and after consulting with my two Radiation Oncologists, I followed their advice. Within six weeks, I started a six month chemotherapy-hormone therapy trial. For me, that did the trick and I have been undetectable ever since. I stopped Lupron/Eligard in February 2010.
Good luck. Listen to a pro and kick the bastard.
Gourd Dancer
In 2007 my PSA went to 7, 16, then 26 every 3 months. My Oncologist suggested 42 radiations. Then my PSA went down to 2.4 for about 4 years, but in 2011 it was at 27 and I had a bone scan. The cancer had metastasized, so I had 30 more radiations, started Lupron, and used Casodex for 6 weeks because of testosterone spikes. I stayed on Lupron (Eligard, generic) for 6 and 1/2 years. In June of this year I stopped Lupron and my PSA has been 0.00 and the Doctor said I am cancer free. Now I am on active surveillance to see if it really is gone. Remember each of us has different cancers, in different parts of the prostate, different insurance, and different Doctors, so we make our own decisions. Ask several doctors and get different opinions.
I was diagnosed in March 2016. PSA 12. Gleason 8.
DaVinci removal in June 2016. First PSA after August .024 . Mid October 2016 before 39 sessions radiation to begin .042. Finished radiation December PSA after .080 (January '17) . Since then I have doubling time of appx 4.2 months. Three body scans nothing. This month 1.70 . No HT yet for me. Now that I'm single digit will re examine after GA68-PSMA this month.
Quality of life to this point was critical factor in his/my decision.
do u realize that the average male carries a psa from 0-4.0 so what are u worrying about. once the gleason score is made then u do treatment immediately but in your case have a drink and relax
When I was first diagnosed by a biopsy, my PSA was 3.4. There are many cases where men with PSA 2.0 are diagnosed with very aggressive cancer and many of them die from their cancer.
If prostate cancer is successfully treated with removal, the PSA should remain undetectable. Even a small increase in PSA indicates there are cancer cells still in the body producing PSA.
After successful radiation treatment, PSA may not become undetectable but should settle down to a small value after a few years.
After my brachytherapy, my PSA went down to 0.1 in two years. But after 5 years it increased to 1.5, when cancerous extra-capsular nodule was detected by another biopsy. When this was treated with cyberknife and ADT, my PSA became undetectable (<0.1) and stayed there for about a year. Then it started quite rapidly. In nine months, it has gone from undetectable to 1.8. The rate at which it is increased, it must have exceeded 2.1 by now. According to acceptable definition of Bio Chemical Recurrence (BCR) of nadir(lowest PSA after primary RT) + 2.0, I have BCR. Now I am going to have Axumin PT/CT scan to find out whether I have clinically detectable cancer. How much I have to worry, would depend on the result of the scan.