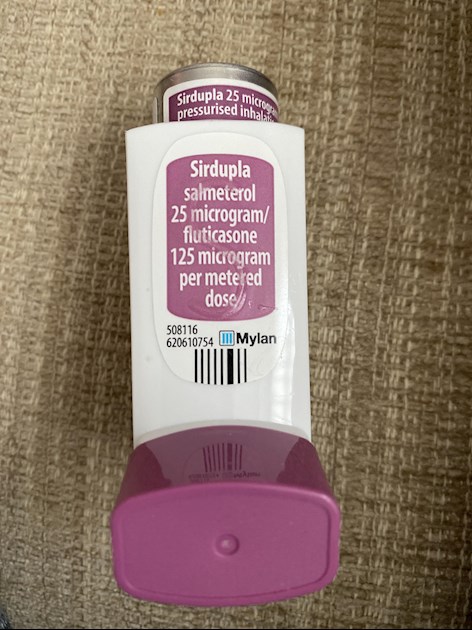
Hi, I’m new hear. I’m a lady in my fifties and have a rare form of dwarfism the syndrome does effect my respiratory and the asthma nurse put me on Sirdupla/fluticasone 3 weeks ago. I have waited for one year to have a full lung function test and sleep apnea test. My peak flow is under 250.
Asthma : Hi, I’m new hear. I’m a lady in... - Living with Asthma
Asthma
I would push for a lung function test. I've already had one this year. You shouldn't be waiting that long. 250 seems low to me. Have you got a releaver inhaler like salbutamol?
Hi Gsp- yes I have a salbutamol. Phone call from Respiratory consultant a year last June, he told me I would probably have test in December 2020 because of the covid I had to wait. I know the syndrome affects the respiratory however, doctors are adamant I have asthma. I’ll phone the nurse and tell her my peak flow is still below 250. Doctors put me on 3 different inhalers back in 2009 and they all failed, I was in severe distress Chest X-ray showed my chest wall was failing so I came off all inhalers then my oxygen level came back up. Still feeling like a weight is on my chest and sometimes burning in lungs when I walk especially at fast pace. Thank you for your message.
Welcome! I hope you manage to get something sorted out.
I don't share your condition (dwarfism) but I do have asthma, COPD and bronchiectasis.
Recently, I've been struggling with my PF which is currently 200, down from 260 (best). I'm on antibiotics for a persistent Moxirella infection and prednisolone.
I found this article the other day and it may be useful to you.
hopkinsmedicine.org/health/...
It told me a lot I already knew but seemed to be clearer, somehow. The bit I found most useful is near the end of the article and talks about Red, Yellow and Green signs and how your PF might relate to them. See what you think.
There is a lot more useful information on the BLF site.
If I were you, I would pester people until I got more help and advice, and, hopefuly, the test you should have had last December. You are as important as everyone else in the queue!
xx Moy
Hi Lilyorky,Welcome to the group! I think you will meet a lot of people with different breathing/lung issues who can share with you their experiences. I am very sorry you had to wait a year for testing. COVID-19 has really changed our world!
What i have learned is that a spirometry lung test is needed to diagnose asthma and other lung conditions. Peak flow monitoring alone doesn't give enough information. I suggest you talk to your doctor about getting Full Pulmonary Function Testing that includes Spirometry, Lung Diffusion and Lung Volumes. That will give them a more definitive look at your lung function. See a lung specialist if you can.
What I have learned is that patients have to advocate for themselves to get answers, don't stop until you get some relief and an answer of how to best manage your condition.
Please keep in touch with us.
Hi Maryhart, thank you for the welcome. It’s awful this covid. I was actually at work when my breathing started to get worse this was in November 2019 so the doctor referred me to a respiratory consultant. I think I was on 16 week waiting list and then the Covid hit. Had telephone consultation June 2020 he said a full lung function test and 6 minutes on a treadmill. He hasn’t heard of my syndrome before and insisted it was asthma and stated it wasn’t the inhalers that failed. My GP misdiagnosed angina so GP sends me to have echo gram. I did see cardiologist. He looked at chest x-rays, MRI of my neck and thoracic, I’ve spinal stenosis and several bulging disc’s. Cardiologist stated It’s not angina my heart is fine, said it’s my spinal issues that’s weakening my chest muscles. When I had my MRI they advised my GP to refer me for spinal surgery. GP decided that surgery wouldn’t help and just to get on with it… I thank you for the advice, it’s much appreciated. I may have to pay private to see a spinal surgeon? I keep you updated.
Wow! You're a walking miracle! Thank goodness those medics got it wrong all those years ago so you are here alive and kicking at the age of 53!I'm sorry to hear that your Dad passed last year. Frontal lobe dementia must have been a difficult thing for him to live with, especially having COPD too. And your sister's got COPD too now. With your lifelong breathing difficulties as well, you must be pretty expert in how the lungs work etc. You can probably tell the nurse a thing or two!
I hope they can get you settled with the right meds. You sound as though you have quite enough to deal with without having asthma on top.
As for me, I'm doing ok at the moment. I think the antibiotics are working, albeit slower than I would like, and today I've had a lot more energy so I feel as though I may have finally turned the corner.
Let us know how you get on with the nurse when you see her. xx Moy
I sorry you are going through this experience. I recommend your asking your doctor to write a referral, if necessary for the Pulmonary Function Testing. With a sleep apnea study, there are some criteria that must be seen or documented. I recommend your asking your doctor to write a referral, if necessary, for you to see a sleep specialist with the criteria.