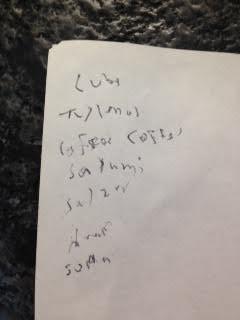
I wanted to see what the effects might be. How soon does the body deteriorate after stopping L-Dopa? I stopped Rytary 9 days ago. I've had two mild bouts of dizziness. And as can be seen on this shopping list my hand writing has gone from bad to worse. I wondered if there might be withdrawal signs. I don't feel any. Obvious question is why stop necessary meds. It's proven that I have PD; My DAT Scan says so. But if I have a deficiency of dopamine then taking a dopamine product prevents the body from trying to make more. Isn't a better method trying to stimulate the body to make more? I'm looking into red light therapy for that reason.
Stopping meds: I wanted to see what the... - Cure Parkinson's
Stopping meds
Hi kaypeeoh. It is dangerous to stop cold turkey like this. You could be hit quite badly with Neuroleptic Malignant Syndrome and it can happen without warning
RKM
Listen to pdpatient. Restart you med schedule. Also start high dose B1
I don't think taking LDopa stops your body from creating dopamine. If LDopa helps then you have a shortage. Be careful.
I stopped and substituted Macuna Prurians, NAC and B1 along with other suppliments on and off but these 3 mainly. did this 3 yrs ago
Which supplements?
My husband stopped several years ago, mainly because he kept forgetting to take his meds and then noticed he didn't feel any different. He took some mucuna sometimes but each time he saw the neurologist, he was persuaded to start taking sinemet again, so eventually he did. However, it made him feel worse, and he started to have freezing episodes which he'd never had before. So he stopped taking it again; but, once more was eventually persuaded by the neurologist to take Madopar instead of Sinemet. He's been taking 50mg 3 times a day for the past 2 or 3 years. This dose seems to agree with him (although he's always in constant pain). He was diagnosed 16 years ago at the age of 51.
You don't have enough healthy neurons to produce enough dopamine to get your body function properly. Ldopa do not make your remaining neurons lazy....you just can't produce anymore a sufficient dose of dopamine because a lot of your neurons are gone. Listen to pdpatient and Roy. it's very stupid what you're doing, sorry to say.
Hi. Love to hear how you get on. Anita
Proof of PD with the DatScan. I wouldn't stop taking the meds. Going cold turkey with any meds can be problematic to one's system. Many meds you need to wean off of them. However, not quite sure why you would want to stop the PD meds.
I'd add supplements which have shown positive results in slowing the progression of PD. Like RoyProp states try the HB1 protocol (read up on it first) and same with Mannitol (read up on it first).
Be safe.
Ji kaypeech
I think you have the wrong idea of what I recommend!
I recommend that we all start doing brisk walking, which I call 'Fast Walking'. Which can only be done SLOWLY over a period of moonths. The goal is brisk walking for one hour, three trimes a week.
My next recommendation is: When you start to feel a lot better THEN start to reduce the medication. The reason for reducing medication is because IT IS ALL TOXIC and it ALL HAS SIDE EFFECTS!
I know that many people either cannot, or do not want to start brisk walking. That is their choice and I can do nothing about it,
For those who do the fast walking and don't feel any benefits within three or four months are either not walking fast enough FOR THEM or their tpe of Pd does not react to the body and brain becoming fitter.
I have lots of people who are doing well with this but seldom hear from those who don't. Thanks for telling me this as it does help to settle the muddy water.
There is an easy test to tell you whether you are walking at YOUR maximum speed That is, while you are walking and you think you are at maximum, then you should not be able to say more than two or three words to a person walking next to you or to yourself. If you cannot speak at all you are going a tad too quickly, bring it down a shade.
If you are doing the brisk walking and you would like to speak to me then contact me at johnpepper@telkomsa.net
John
John, I've enjoyed reading your story, so let me share mine:
I've been fast-walking for over 50 years! I started as an 11-year-old with an after-school paper route. It was the largest route in town (140+ customers). The houses were close together and I had to put the papers inside the door or in the mail slot, so I couldn't ride a bike to do it. I had to walk. I always hurried because I wanted to get home in time to watch Star Trek re-runs. I had that route for 7 years and was probably the oldest paperboy ever because I liked being my own boss and loved walking. Working for minimum wage at a burger joint just didn't make sense to me. Everyone else probably thought I was a little nuts.
Then I worked for the US Postal Service for a few years, delivering mail and going to community college. I would walk (or ride a bike) to the PO to pick up my mail, drive a PO Jeep out to the route, deliver the mail on foot (much faster than the other carriers), then walk to the college and attend a couple of classes. The hardest part was walking home during a snowstorm at night (this was in Iowa). I didn't even own a car until I was 21. By the time I quit the PO and got a job as a programmer in much warmer California, the habit was so ingrained I almost always either walked or biked to work for the next 30+ years.
So, how did I get PD? I never smoked or drank heavily, but the one bad habit I had was drinking a lot of diet coke. As a programmer, there were a lot of late nights and a lack of sleep. For decades, I drank at least 32 oz per day (most of the places I worked had free cokes) and I'm convinced that the fake sugars they use in soft drinks did a job on me.
About 12 years ago I was diagnosed, but I kept working for 4 more years, always riding my bike or walking (but still drinking diet coke without realizing what it might be doing to me). 8 years ago I retired and stopped walking (also without thinking about it). I got a bit depressed and started deteriorating quickly. I won't go into detail, but I would guess that I was within a year of being bed-ridden for the rest of my life. The realization that I was rapidly headed towards "the end" as some here like to put it, jolted me out of the fog I'd been lost in.
I wanted to walk again. The urge to walk again was very strong. It occurred to me, somehow, that walking had been the key to my good health and could be again. My new-age friend says that I "listened to my inner healer". Maybe. So I started walking just 20 feet outside, then 40, then 100 feet up and down a hill. At first, it was very, very hard. I didn't have the energy to do it, so I also changed my diet, cutting out processed junk, refined sugar, etc. This was 5 or 6 years ago and I still cringe when I think about how poor my condition was back then.
Today I walk very quickly, up and down the hills near Yosemite where I live. I alternate between 1/4 miles and 2 miles a day. It's what works best for me. I also do a little Qigong, light weight lifting, yoga, etc. But nothing helps as much as the walking. I'm almost 64 and was diagnosed at 52. There are times when I feel so good, I do crazy things like skipping and running as fast as I can, and even spin around as I walk. Not always, but quite often. Again, I suppose the neighbors think I'm a bit nuts. That seems to be my lot in life. No, I haven't been able to reduce my meds, but they've stayed nearly unchanged since "the change" as my wife calls it (yes, she calls something else that too, but this is my change and that's her change). I am also trying the red-light therapy with a Coronet Duo. I keep trying new things, but walking has gotten me this far.
That's my story and I'm sticking to it!
Hi Jas9. May I suggest that you should not do high intensity exercise every day. Your body needs time to recover!
To get the best results from walking, it must be sustained for a period of time you can manage and not have any stopping or slowing down. You altaedy know that you have to builod iup to maximumspeed and distance. If you want to be sure you are walkingn at your maximum speed just try this test: Ifv you can say more than three words while walking then youm are not wlaking as fast as you are able to do, If you cant say one single word ytou are going too fast! With your walking, the goal should be one hour every second day. Do other exercise on other days but not on walking days. Try to exercise other parts of your body on the intervening days.
It is your choise! Getting fit is different to getting better with Pd.
Hi John et al,
3 days a week I do an HIIT workout. I follow Dr Mercola's protocol. But on a treadmill. A lot of people say it can lead to injury, including Dr Mercola. But stubbornness is my best feature. It got me through 9 years of college.
I have a new treadmill that's set up for HIIT workouts. I used my old one for ten years. Mercola's method is ten 30-second sprints at 10% incline and 10 mpm pace. With 90 second rest periods between each sprint. On the old machine they were difficult but doable. Heart rate was always 90% of max by the end of each sprint. But on the new treadmill it's been impossible to do the same workout.
Yesterday I tried the workout but nearly got tossed off at the end of the final sprint. I finished safely but PD has made me paranoid about falls.
So I think my problem is white-coat syndrome. It would explain a lot.
Hi Kayspech.
You might find this hard to believ, but it is true:
Sustained fast walking on an uneven surface, like a school playing field, has the most affect on the brain, which is what we need! I know, weather and temperatures do not necessarily allow us to do this. But when we can we should be doing it to get the most out of our efforts.
It is difficult to create the " Fight or Flight" effect on a treadmill or other machines because they do not engage the brain. I have seen people on treadmills watching TV. If they can do that then their brain is not engaged at all.
It is your decision as to what you do to reverse your symptoms, I can only advise..
Kindest regards
I understand. If every foot step has the potential for falling or tripping you have to keep focus rather than daydreaming. Every injury I ever had in races was because of not keeping focus; Lots of skinned knees , cracked ribs and one fractured ankle.
What JohnPepper just said makes perfect sense. Yogis and Qi Gong masters will tell you that PwPs live in their head. They have forgotten their very body and the latter has been violently reacting since the onset of the dys-ease. Knowledgeable psychologists will tell you that it’s all about Dissociation (important keyword). This is confirmed by many MDs who invite you to reconnect with your body and even talk to your body. So, John Pepper’s way of conscious (another keyword of utmost importance) brisk walking can be construed as a form of Yoga or Qi Gong.
***
« Connect with your physical body. Most of the time our attention is outside of ourselves, and we lose awareness of what’s happening inside. This strengthens our belief systems, triggers the amygdala more easily, and keeps us disconnected from what’s really going on. When we bring our attention back to our physical body, we immediately connect with what’s actually happening here and now; the truth, versus what the mind thinks is happening. Just feeling the physical sensations of your feet on the floor or butt on the seat brings your attention out of the mind and allows stress hormones and inflammation to decrease. » (Dr D'Eramo)
***
« Talk to your body. Your cells are listening (1) , and according to your inner system, the leading authority on everything is you! Studies have shown that when you listen to your own voice, it has a far stronger impact on your subconscious thoughts and beliefs than when you listen to anyone else. That means every time you repeat “I’m not okay” or “I can’t get through this” you believe it! Use this power instead to strengthen your body […] » (ibid.).
***
(1) See also : Pr Robert Naviaux, Metabolic Features of the Cell Danger Response. Mitochondrion 2014.
This is a recent article along these same lines:
salon.com/2021/08/28/walkin...
A quote:
What is the connection between walking and thinking...? You may have heard by now how walking makes us feel good by releasing endorphins, lowers risk our of depression; increases cognitive functioning; strengthens memory; enhances creativity; and produces a protein essential for neuronal development and survival, synaptic plasticity, and cognitive function.
Thank you so much Resano for sharing this wisdom. I am going to get on this meditation train.
Coincidentally, I am trading e-mails with a very nice researcher in China (I was asking about their sodium butyrate study) and they are very much encouraging me to meditate and thinks it will improve my health. They said "meditation is a very good method to improve body health, as you know, neuro-endocrine-immunology is the most powerful axis for our healthy states, meditation has been proved improve this axis efficiently" and they have been meditating an hour a day for the last year and a half.
There are so many nice people offering great advice. Thank you.
Exercising - cycling - walking - swimming - boxing - all these will help.
Hi kpo:
"Obvious question is why stop necessary meds. "
IMHO, if your meds provide no benefit, you should not take them, but this should be discussed with your doctor, and done safely.
Note: I don't think I have ever hear of a "hidden benefit" to taking c/l.
I understand it may benefit your handwriting, and depending on your situation, that might justify you taking c/l (it is a personal decision).
Regarding your DATSCAN, some do not think this is conclusive that you have "Idiopathic Parkinson's Disease". Ie, it is not a supporting criteria (but is an exclusionary criteria; see the following reference).
Parkinson’s Disease: Pathogenesis and Clinical Aspectsncbi.nlm.nih.gov/books/NBK5...
Table 1 The clinical diagnostic criteria for Parkinson’s disease, based on the Movement Disorder Society guidelines
Diagnosis of parkinsonism
Bradykinesia
Plus one of
Tremor
Rigidity
Exclusion criteria
Cerebellar abnormalities
Supranuclear gaze palsy
Diagnosis of behavioral variant of frontotemporal dementia or primary progressive aphasia within 5 years of disease onset
Parkinsonian features restricted to the lower limbs for more than 3 years
Treatment with a dopamine receptor blocker or dopamine depleting agent consistent with drug-induced parkinsonism
Absence of a response to high-dose levodopa despite at least moderate disease severity
Cortical sensory loss, clear limb ideomotor apraxia, or progressive aphasia
Normal functional imaging of the dopaminergic system (“DAT scan”)
Diagnosis of alternative condition causing parkinsonism which could be causing the symptoms
Supportive criteria
Clear beneficial response to dopaminergic therapy
Presence of levodopa-induced dyskinesia
Rest tremor of a limb
The presence of either olfactory loss or cardiac sympathetic denervation on MIBG scintigraphy (although the latter is rarely done in current practice)
Red flags
Rapid progression of gait impairment leading to wheelchair use within 5 years
Absence of progression of motor symptoms over 5 years, unless related to treatment
Early bulbar dysfunction
Inspiratory respiratory dysfunction
Severe autonomic failure within the first 5 years of disease
Recurrent falls because of impaired balance within 3 years of onset
Disproportionate anterocollis or contractures within 10 years of disease onset
Absence of any of the common non-motor features despite 5 years of disease
Unexplained pyramidal signs
Bilateral symmetrical parkinsonism
For the diagnosis of clinically established PD
Parkinsonism
Absence of exclusion criteria
At least 2 supportive criteria
For the diagnosis of clinically probable PD
Parkinsonism
Absence of exclusion criteria
Balanced numbers of supportive criteria and red flags
Note: A supportive criteria is "A clear beneficial response to dopaminergic therapy".
ARRRGGGHH! A long, drawn advertisement. Had to listen to most of it before finding it's an ad for Jodi Knapp's protocol. I remember looking into that last year and found nothing useful. ARRRGGGHH!
Please don’t go cold turkey. I did and experienced Neuro malignant syndrome. It can kill u!!!
All I can say, is that it is really important, that you check with your neurologist/physician/movement disorders specialist, before you stop Carbo/levodopa treatment, cold Turkey, like that. Perhaps you did. If not, though, it would be wise to check, with a professional specialist, because there are side effects, that could occur, stopping cold Turkey! Hope you achieve the relief, you are looking for!