A very interesting paper.
Difficult to grab any individual bits for discussion or introduction. The whole paper isn't very long.
Even if bipolar disorders are not themselves of much direct interest, it might be worth a quick read because it discusses the control group as well and their ability to tolerate these high doses (300 micrograms a day - and much higher).
Note that the mention of valproate avoidance has now (since publication of this paper) extended to include males - and is very important.
The authors are all based in the UK.
A new approach for the treatment of subthreshold bipolar disorders: Targeted high dose levothyroxine and repetitive transcranial magnetic stimulation for mitochondrial treatment
Andy Zamar 1 Abbi Lulsegged 2 Christos Kouimtsidis1,3*
1 Consultant Psychiatrist, The London Psychiatry Centre, London, United Kingdom
2 Consultant Endocrinologist Health 121 Ltd., London, United Kingdom
3 Honorary Senior Lecturer Imperial College London, London, United Kingdom
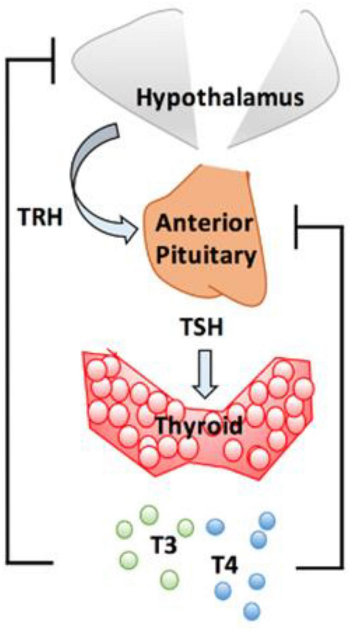
Bipolar spectrum disorder includes Bipolar I, Bipolar II and subthreshold bipolar disorders (BD). The condition is highly prevalent, disabling and associated with high mortality. Failure of diagnosis is high. Subthreshold presentations present as 4 or more changes in polarity, are generally less responsive to standard treatment and as a result, drug combinations are often needed. High Dose Levothyroxine (HDT) has been reported to be safe and effective with this condition. Treatment response has been associated with mutations in thyroid activating enzymes and intra cerebral transporter protein carrier. Repetitive Transcranial Magnetic Stimulation (rTMS) has been shown to be effective in bipolar depression and has been proved to have neuroplastic effect. Present authors had reported clinical evidence of safe and effective use of a combination treatment protocol. Potential mechanisms of action of the combined treatment protocol and the role of mitochondria function are discussed.
Open access here:
 Just can't wrap my head around it.
Just can't wrap my head around it. 