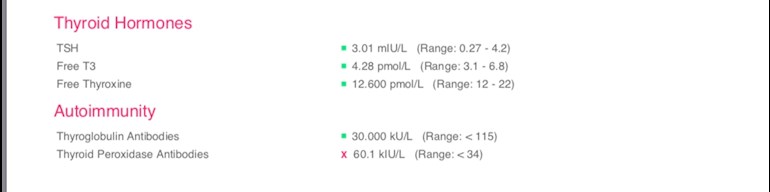
I recently decided to get some bloods checked with Medicheck. Having raised autoimmune levels, is this anything to be concerned about? I seem to be in normal range for the other results. After suffering for years with a fast heart rate which could come on whilst sat watching tv (highest 174bpm) this was always put down to anxiety by my doctors, I almost give up visiting them on ocassions. Could my levels still say normal but get symptoms?
Out of range Thryroid Peroxidase Antibodies - Thyroid UK
Out of range Thryroid Peroxidase Antibodies
I cannot read your results very well.
If we have thyroid antibodies in our blood we have a condition called 'Autoimmune Thyroid Disease', commonly called Hashimoto's. Treatment is the same as for hypothyroidism.
Going gluten-free can help reduce the antibodies and the attacks but you will become hypothyroid.
thyroiduk.org.uk/tuk/testin...
thyroiduk.org.uk/tuk/about_...
thyroiduk.org.uk/tuk/about_...
When you have a blood test, it should always be at the earliest, fasting (you can drink water) and allow a gap of 24 hours betwen last dose of levo and the test and take afterwards. This helps keep the TSH at its highest. Always get a print-out of your results with the ranges.
You should also check B12, Vit D, iron, ferritin and folate. All have to be optimal.
If you're in the UK, we aren't diagnosed until the TSH reaches 10 (hypothyroidism) whilst in other countries we'd be if it reaches 3+).
However, if antibodies are present, regardless of the TSH you should begin on levothyroxine at 50mcg and have blood tests every six weeks thereafter until TSH is 1 or lower.
I can't read your results at all I'm afraid, and don't know to which antibodies you refer. If you delete the photo from the post, edit it to remove all but the key information, then upload it again, it is likely to be much clearer.
Your raised TPO antibodies indicate that you probably have an autoimmune condition, commonly known as Hashimoto's disease, which can attack the thyroid gland, and cause it to fail. An important point is that having a blood test result that is anywhere within the reference range, doesn't mean it is "normal", only that it is the same as some of the people who were originally tested to arrive statistically, at a bell curve of results, and who may themselves, have had some degree of thyroid dysfunction. So your results may not be optimal for you - which is a good possibility since your FT4 level is scraping along at the bottom of the range. Many of us might expect to see our FT4 in the upper half of the range when we feel well, so with that range, that would be above 17.0, although we are individual in what helps us to feel well, or causes us to feel unwell. Proportionately, your FT3 result is slightly better than your FT4, but nevertheless, is low in range - we might generally expect to feel better with a FT3 in the upper quartile. So it seems that your thyroid is beginning to show the effects of you having the autoimmune condition, and could explain your symptoms, although many Drs wrongly assume that it is only an excess of thyroid hormones that causes heart racing, palpitations, AF etc. Additionally you may be showing the effects of nutritional deficiencies - have you been tested for Vit D, Vit B12, ferritin and folate for starters? With your results being "in range" it's less likely a Dr will initiate treatment for your thyroid, and there is no medical treatment for Hashimoto's although some people initiate lifestyle changes such as excluding gluten and/or dairy for instance, which may help, although not for everyone. However, as your FT4 level is very low, and you have elevated antibodies in addition to your longstanding symptoms, it is worth showing these results to your GP and asking to be started on a trial of Levothyroxine.
TSH is too high for someone with Hashimoto's, whatever the reference range says! As others have said, T4 is at bottom of range and T3 is also rather low. Everything needs to be optimal.
It means that you have autoimmune thyroid disease (aka Hashimotos) which will gradually destroy your thyroid. Already your free T4 is at the bottom of the range and your TSH is showing that your thyroid is struggling to produce enough free T3 to keep you functioning. However, the NHS will not treat until you have really bad symptoms and over range TSH, or TSH goes over 10. As the thyroid is destroyed, it releases excess hormones into the blood stream causing hyper symptoms like sweats and high heart rate, then you become more hypo and get cold, tired and constipated etc. That continues until the thyroid is dead. You can get adrenaline rushes and high heart rate even when in a hypo phase as the body produces extra adrenaline to keep you going and make up for the low thyroid hormones
Recommended on here that all thyroid blood tests should ideally be done as early as possible in morning and fasting. This gives highest TSH, lowest FT4 and most consistent results. (Patient to patient tip, best not mentioned to GP or phlebotomist)
Is this how you do your tests?
Your TSH is on high side, FT4 is very low and FT3 not brilliant
This combined with high antibodies shows you are "subclinical hypothyroid " by official guidelines
Almost certainly need trial of Levothyroxine
thyroiduk.org.uk/tuk/about_...
SeasideSusie has a link about getting GP to consider 3-6 month trial of Levothyroxine in this situation
Essential to test vitamin D, folate, ferritin and B12
Ask GP, or get Medichecks to test
Very likely some of these will need supplementing to improve
Hashimoto's affects the gut and leads to low stomach acid and then low vitamin levels
Low vitamin levels affect Thyroid hormone working
Poor gut function can lead leaky gut (literally holes in gut wall) this can cause food intolerances. Most common by far is gluten. Dairy is second most common.
According to Izabella Wentz the Thyroid Pharmacist approx 5% with Hashimoto's are coeliac, but over 80% find gluten free diet helps, sometimes significantly. Either due to direct gluten intolerance (no test available) or due to leaky gut and gluten causing molecular mimicry (see Amy Myers link)
Changing to a strictly gluten free diet may help reduce symptoms, help gut heal and slowly lower TPO antibodies
Ideally ask GP for coeliac blood test first or buy test online for under £20, just to rule it out first
Trying gluten free diet for 3-6 months. If no noticeable improvement then reintroduce gluten and see if symptoms get worse
chriskresser.com/the-gluten...
amymyersmd.com/2018/04/3-re...
thyroidpharmacist.com/artic...
scdlifestyle.com/2014/08/th...
drknews.com/changing-your-d...
restartmed.com/hashimotos-g...
But don't be surprised that GP or endo never mention gut, gluten or low vitamins. Hashimoto's is very poorly understood
Hi thank you for your reply. This is the first time I’ve used Medicheck for blood tests, I’ve had two previous blood tests through my GP, both have had previously raised Thyroid Peroxidase Antibodies. But they’re suggesting my results are “normal” and no treatment is needed, just regular bloods to catch it at the best time, I’m guessing once this happens it won’t feel like the greatest of times for me! This test was done first thing in the morning and fasted. I also don’t eat gluten, I’m on a strict healthy diet, as I like to train in the gym quite a bit. I’ll certainly look into getting some other checks done, in the hope I can move forward with this somehow before it reaches a pretty desperate stage. The doctors tell me I shouldn’t be having any symptoms, I’m pretty in tune with my body and I can definitely say I am, in their eyes though... what do I know 🤷🏼♀️
Mrs_MacMurray
With regard to raised antibodies and a diagnosis/trial of Levothyroxine, TSH needs to be over range for this to be considered. If you can get a result where TSH is above range and antibodies positive then you can use Dr Toft's article in Pulse magazien (the magazine for doctors) where he said in answer to Question 2:
Question 2 asks:
I often see patients who have an elevated TSH but normal T4. How should I be managing them?
Answer:
The combination of a normal serum T4 and raised serum TSH is known as subclinical hypothyroidism. If measured, serum T3 will also be normal. Repeat thyroid function tests in 2 or 3 months in case the abnormality represents a resolving thyroiditis.
But if it persists then antibodies to thyroid peroxidase should be measured. If these are positive - indicative of underlying autoimmune thyroid disease - the patient should be considered to have the mildest form of hypothyroidism.
In the absence of symptoms, some would simply recommend annual thyroid function tests until serum TSH is over 10mU/l or symptoms such as tiredness and weight gain develop. But a more pragmatic approach is to recognise that the thyroid failure is likely to become worse and try to nip things in the bud rather than risk loss to follow up.
Treatment should be started with levothyroxine in a dose sufficient to restored serum TSH to the lower part of it's reference range. Levothyroxine in a dose of 75-100mcg daily will usually be enough.
You can obtain a copy of the article by emailing Dionne at
tukadmin@thyroiduk.org