In Professor Sir Bruce Keogh’s vision for urgent and emergency care, people who ask for care will be treated at or near their homes, maybe over the phone, whenever this is clinically the right thing to do. Only those in urgent need of hospital resources will go to an emergency centre for treatment. You can read more about the Urgent and Emergency Care Review here:
nhs.uk/NHSEngland/keogh-rev...
Making this happen will improve patient care. By reducing patient pressure on hospitals, it could lower the overall costs of urgent and emergency care as well.
Connecting the dots
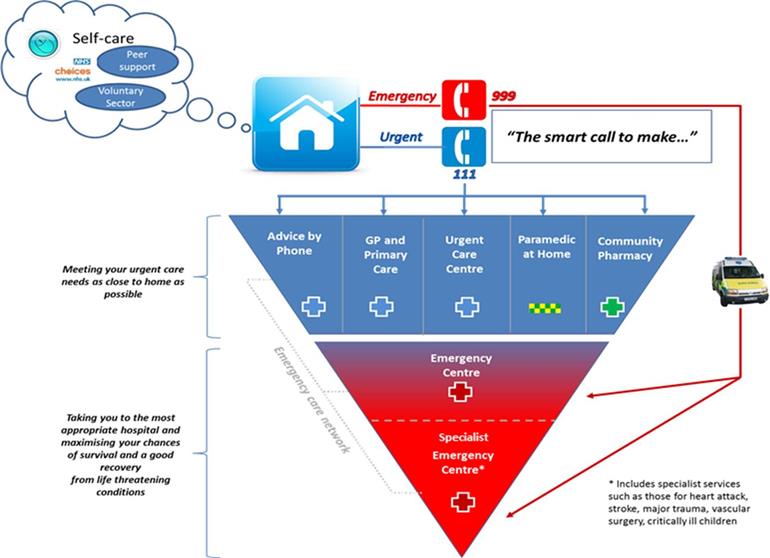
Realising the vision of the Urgent and Emergency Care Review depends on connecting all the services that currently provide urgent and emergency care – and their commissioners – into a single system (see image). They all need to co-ordinate their capacity planning and operations to make sure each patient is directed to the right setting and gets the right treatment on his or her first call for urgent help.
That kind of joined-up working has been hard in the past, partly because all the players in the system get paid for what they do in different and uncoordinated ways. At the moment, reimbursement to hospitals and urgent care centres for urgent and emergency care is almost entirely activity-based, while GPs and other providers of urgent care close to home are mostly paid through block contracts. Some hospital providers could be at risk of reduced income from shifting urgent and emergency care closer to home, even if it would unclog bottlenecks or free up resources in the system overall. Hospitals do have to cover the fixed costs of having capacity ‘always on’ and are heavily dependent on activity to achieve this. Even when trying to work collectively in a wider health economy, this can act as a financial disincentive.
Focus on patient benefits
Monitor and NHS England, together with local services and commissioners putting urgent and emergency care systems in place, are working on how to align patient benefits and service providers’ financial incentives in urgent and emergency care payment arrangements. We think the way forward could be a single, consistent payment approach for every type of service in the system, made up of 3 elements:
1. The first element would be substantial and fixed, to reflect the ‘always on’ nature of urgent and emergency care. This would help to concentrate commissioners and service providers on co-ordinating capacity planning in line with expected changes in patient flows.
2. The second element would be volume-based and variable, to limit the impact of unpredictable fluctuations in demand on individual providers across the system. This element would also help to allocate volume and cost risk to support the kind of co-ordinated behaviours that will realise the vision of the Urgent and Emergency Care Review.
3. Each of these 2 elements could be available at different levels or rates of payment. So the third element of the approach would be to measure the quality of individual providers and of the system as a whole and use these quality measures to determine a provider’s eligibility for their particular level and rate of payment. These measures could also be the basis for bonuses and penalties.
An urgent and emergency care payment approach with these features would allow individual providers to see some financial benefit from any steps they take that help realise the aims of the Urgent and Emergency Care Review but which are not in their immediate individual financial interest. For instance, ambulance services could be rewarded for providing more care on scene with support from hospital consultants, reducing the need for hospital treatment; hospitals could receive a share of the system gain from this measure as a quid pro quo for providing access to the experts.
We need your input
We’re a long way off a detailed proposal for a single, consistent approach to urgent and emergency care payment across the system. The concept raises a lot of questions. How can quality and financial costs and benefits across the system be counted? Who should keep the account and manage the payment flows? How could the new approach be implemented?
We’re keen to know what providers and commissioners think of the concept, and of the many questions it raises. If you and your organisation would like to get involved, please write to pricing@monitor.gov.uk or england.paymentsystem@nhs.net. A great start would be to answer the consultation questions in our document detailing the concept by 9 September, which can be accessed here:
gov.uk/government/consultat...
Getting payment for urgent and emergency care right is crucial to making the vision a reality.
Jyrki Kolsi is pricing development lead at Monitor.