While I normally attach study links to my posts with a basic explanation and possibly a quote or two from the study, I have made a decision not to do that in this particular post in order to try and make the post a bit shorter, in the hope that more members will read it as I feel this is potentially an important message which I want as many members as possible to be aware of for its potential to fix the broken gut microbiota without FMT.
I've discussed melatonin at length on this forum as well as Short Chain Fatty Acids(SCFAs) including butyrate, but I have not previously discussed Peroxisome proliferator-activated receptor gamma or PPAR-y (PP-y). In a video that Bolt_Upright was kind enough to post (thank you!) on Saturday (07-10-2021), Lucy Mailing, PhD, discussed PP-y and described it as a "master switch" to initiate repair of the gut microbiome and went on to describe a dozen or so methods of increasing PP-y using supplements, herbs, CBD etc. Her suggestion was to consider these known increasers/agonists of PP-y either alone or in combination to try and increase PP-y enough to have that effect of increasing PP-y. I had not previously heard of PP-y as useful in terms of gut repair, but she was certain about its effects. So it made me do a little digging since I have always been interested in the gut microbiome and that interest has increased exponentially with the results of the FMT/PD studies from 2020 and 2021 which saw significant improvement in multiple PD test scores as well as motor and non-motor symptoms in PwP. What these studies suggested is that gut dysbiosis is a major contributing cause to PD symptoms. Here is a link to her video as it is the basis for this post.
The thing I was wondering about from her video is that Dr. Mailing chose to use substances that are not native to the body to try and increase PP-y. My thinking is that it might be another option to consider a molecule that is not only native to humans and animals, but plant life also and is known to be healthful in all three instances of application. Dr. Mailing also discussed the important role of inflammation and oxidative stress in fueling the fires of gut dysbiosis, but her focus was directed more at the inflammatory aspect of gut dysbiosis. So it would be quite useful if this same molecule could also have potent antiinflammatory and antioxidative stress effects in the gut, and fortunately this molecule does exactly that. Another issue that Dr. Mailing noted as a result of dysbiosis is excessive mitochondrial stress that she said would also need to be addressed and again this molecule is very protective of the mitochondria and in fact is produced in the mitochondria.
To be clear, the molecule I am describing is Melatonin and what her video did was to motivate me to look even closer at melatonin to see if it is likely to have even more benefits for PwP than I have mentioned in my many previous posts on this forum about melatonin and its many healthful benefits. I decided to make a list of some of the benefits of melatonin that I have not previously mentioned. Here are the important items that I found that can be added to that list of potential melatonin health benefits.
1. Melatonin increases PP-y at the gene level and according to Dr. Mailing, this is a very important step in initiating repair of the gut microbiota.
2. Previously I have mentioned that butyrate can increase melatonin production in the gut, but I only recently found out that melatonin can not only increase Short Chain Fatty Acids (SCFAs) including butyrate, but it can also increase butyrate producing bacteria in the gut microbiota and this is very important because PwP are low in the 3 dominant SCFAs as well as the bacteria needed to increase SCFA production and butyrate in particular. The other two dominant SCFAs are Acetate and Propionate. Of these three, propionate is the lowest in PwP. This is only a recent PD mouse model study, but in it, it was shown that increasing the propionate level could also improve motor symptoms in these mice.
3.Another point that Dr. Mailing said needed to be dealt with in order to functionalize gut repair was to reduce Proteobacteria in the gut and again melatonin has shown the ability to modestly reduce this bacteria.
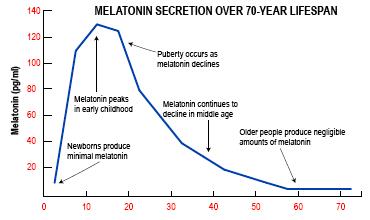
4. I have often wondered about the role that SCFAs, Acetate and Propionate play in the gut microbiota and interestingly, they have shown the ability to increase melatonin receptors in the gut and in conjunction with the fact that butyrate increases melatonin production in the gut seems to add further credence to the importance of melatonin in the gut microbiota. Also keeping in mind that production of melatonin in studies was shown to be anywhere from 400 to 1000 times as high as what is produced by the pineal gland which seems to further highlight the importance of melatonin in the gut. Add in the potent antioxidative stress and antiinflammatory effects that melatonin has shown in many studies and a clearer picture of the importance of melatonin in the gut microbiota is starting to emerge. It is also important to remember that melatonin declines with age, conversely to how age related diseases increase with age. PD is an age related disease and advancing age is the number one risk factor for getting PD. PD and its symptoms are enhanced and advanced by excess oxidative stress and inflammation and returning these two features to normal levels, imo is like starving the disease. This is essentially what FMT does, returns the gut microbiota to a more normal state where oxidative stress and inflammation are very well controlled and clearly was beneficial for PwP in the FMT studies.
5. Both melatonin and butyrate repair the gut mucosal barrier function as well as protect the epithelial cells against inflammation which is very important for the purpose of reducing or preventing leaky gut and improving gut barrier function as a means to reduce inflammation and oxidative stress associated with gut permeability. Together they have synergy and health promoting effects as the gut microbiota seems to be an important determining factor in whether we are healthy or not.
6. Another issue that Dr. Mailing said that needed to be addressed in terms of gut repair was Mitochondrial oxidative stress. Interestingly melatonin is produced in the mitochondria and can apply its potent antioxidative stress and antiinflammatory qualities in a timely manner to neutralize oxidative stress almost instantly and mitochondria can also draw melatonin into the mitochondria if there is ample melatonin available around the mitochondria, but if butyrate increases melatonin production and butyrate is very low, melatonin levels in the gut may decline to levels that are insufficient for melatonin to be able to apply all of its protective effects in the gut microbiota and mitochondria. I believe melatonin is one of the main reasons that PD can take one or two decades to show symptoms enough to actually have a diagnosis because melatonin is doing such a good job of controlling inflammation and oxidative stress while protecting dopaminergic neurons and mitochondria in the brain. With the age related decline of melatonin, PD and its accompanying chronic inflammation and oxidative stress, melatonin and SCFAs eventually begin to lose their ability to protect the gut microbiota. Possibly, repairing the gut biome via increased melatonin and SCFA may improve disease symptoms significantly as illustrated by the FMT / PwP studies that repair and rebalance the gut flora back to levels of healthier bacterial balance between pathogenic bacteria and health promoting bacteria.
7. This one is going to be a leap of faith and is pure speculation on my part. I was not previously aware that melatonin increases butyrate and butyrate increases melatonin. We are all mostly aware that inflammation creates oxidative stress and in turn oxidative stress creates more inflammation in a repetitive negative cycle that tends to destroy health and create health issues of all types as well as fuel many disease states such as PD,AD and MS to name only a few. Have you ever wondered if there is a similar effect that is "pro-health" instead of "anti-health"? I have! I'm trying to understand this intimate relationship between these three dominant SCFAs and melatonin and if I am seeing this correctly it is the closest thing I have seen to a health promoting positive repetitive cycle. Butyrate as well as acetate and propionate have multiple health promoting effects in the gut and the butyrate increases melatonin. Melatonin has health promoting effects throughout the body and specifically in the gut and it increases butyrate. Acetate and Propionate increase melatonin receptors in the gut. As SCFAs and melatonin increase in this repetitive cycle, theoretical repair of the gut biome would be expected based on the available science and based on these known activities, this cycle should continue until the gut biome is returned to homeostasis and from there overall health body wide should follow. Pretty much the reverse of what is seen once excess oxidative stress and inflammation are allowed to advance unabated, the gut biome goes into a state of dysbiosis followed by a general decline in health followed by disease, general ill health and ultimately a potentially premature death. So this idea of a potential healthful cycle is new to me and I have not previously thought that there was a healthful cycle that could be the healthful version of the unhealthful oxidative stress/inflammation cycle, but melatonin and SCFAs could very well be it! In PD, SCFAs as well as SCFA producing bacteria are depleted as well as melatonin in the gut and brain, so this gives an idea of how this positive health cycle could be quite beneficial in PwP.
So in my opinion, the molecule she failed to include in repairing the gut microbiota is melatonin, because it simply checks most of the boxes that she said needed to be checked in order to repair the gut microbiota and it is naturally occurring in the body and gut in particular in large amounts and has protective effects throughout the body. It also seems to have synergy with SCFAs and butyrate in particular and may be of very significant importance in promoting a positive health cycle where SCFAs feed off of melatonin and melatonin feeds off of SCFA to continuously promote repair of the gut microbiota and the body as a whole.
I am putting this theory out there for your consideration because it is the best understanding I have been able to determine from what I know about melatonin and SCFAs so far. If the theory is correct, then it should be able to essentially replicate what FMT has shown to do in PwP. While FMT is currently available for a handful of health issues, it is not yet available for PD. As such, this healthful cycle theory may be an available option worth considering now for having a potentially similar impact as FMT. An important point to keep in mind is that I have not seen any other adjunctive treatment that can improve PD symptoms and test scores anywhere close to what FMT does and it is likely to improve overall health.
Art
 Jim
Jim