Living with Stage 4 Chronic Kidney Disease
- 0About this program
- 1What Is CKD and What Can I Do?
- 2Testing and Management
- 3Protecting Your Kidney Health
- 4Coping: Handling Emotions and Stress
- 5Protecting Your Heart If You Have CKD
- 6Good Nutrition and Kidney Disease
- 7Making Healthy Lifestyle Choices
- 8Managing Complications of Advanced CKD
- 9Treatment of Kidney Failure
- 10Understanding Kidney Transplantation
- 11Understanding Dialysis
- 12Working With Your Healthcare Team
- 0About this program
- 1What Is CKD and What Can I Do?
- 2Testing and Management
- 3Protecting Your Kidney Health
- 4Coping: Handling Emotions and Stress
- 5Protecting Your Heart If You Have CKD
- 6Good Nutrition and Kidney Disease
- 7Making Healthy Lifestyle Choices
- 8Managing Complications of Advanced CKD
- 9Treatment of Kidney Failure
- 10Understanding Kidney Transplantation
- 11Understanding Dialysis
- 12Working With Your Healthcare Team
Content on HealthUnlocked does not replace the relationship between you and doctors or other healthcare professionals nor the advice you receive from them.
Never delay seeking advice or dialling emergency services because of something that you have read on HealthUnlocked.
Understanding Dialysis
What is Hemodialysis?

Dialysis is a treatment option when your kidneys fail – meaning they are no longer able to do their job to keep your body healthy. There are different types of dialysis. Dialysis can be done at home or in a clinic. It can be done during the day or at night. It is important to learn about all your options so that you can find a treatment option that works best for you and your family.
Hemodialysis is a treatment that removes wastes and extra fluid from your blood. During hemodialysis, your blood is pumped through soft tubes to a dialysis machine where it goes through a special filter called a dialyzer (also called an artificial kidney). Smaller waste products, such as urea and creatinine, and extra fluid, move from your blood through the membrane, and are removed. As your blood is filtered, it is returned to your blood stream. Only a small amount of blood is out of your body at any time.
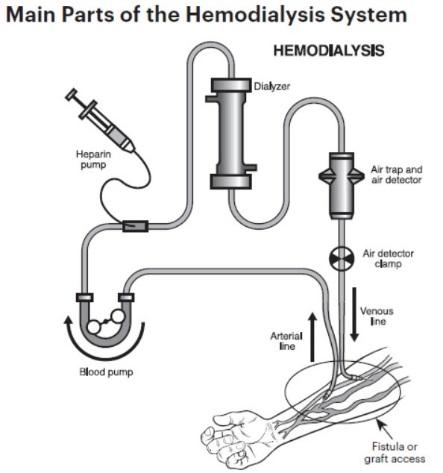
To get your blood into the dialyzer, you will need an access into the bloodstream for placing needles needed for hemodialysis into your blood vessels. This is done with minor surgery, usually to your arm.
You can watch the following video for more information on hemodialysis.
Understanding dialysis access and vein preservation
With hemodialysis, to get your blood into the dialyzer, you will need an access into the bloodstream for placing needles needed for hemodialysis into your blood vessels. This is done with minor surgery, usually to your arm. Types of access include:
Fistula: A fistula is the recommended choice for an access. It is made by joining an artery to a nearby vein under your skin to make a bigger blood vessel. This type of access is preferred because it has fewer problems and lasts longer. However, some people may not be able to have a fistula because of their physical condition.
Graft: If your blood vessels are not suitable for a fistula, a graft may be used. This involves joining an artery and a nearby vein with a small, soft tube made of synthetic material. The graft is entirely beneath your skin.
Catheter: The third type of access, called a catheter, is inserted into a large vein in your neck or chest. The ends of the tubes sit on your skin outside your body. This type of access is generally used when you need dialysis for a short period of time. Catheters are used as a permanent access when a fistula or a graft cannot be placed.
If you choose a fistula, you may need to discuss the issue of vein preservation with your healthcare team. This is done to make sure parts of your arm are available to surgically create an access for dialysis. For example, this can involve informing all clinicians about your situation and the need to protect certain parts of your arm. This is to make sure that certain parts of your arm are not used for blood draws or intravenous needles, unless it is an emergency. You might also need to plan ahead for a fistula placement, preferably 6-12 months prior to the estimated need for hemodialysis, which allows time to conduct the surgery and for the fistula to mature.
Considering in-center versus home dialysis
There a number of issues to consider when deciding on a type of dialysis, including where to receive treatment. This is an important consideration that should be made between you, your family and your healthcare team. You can do hemodialysis at a dialysis center where a nurse, technician, or other member of the healthcare team performs the tasks required during treatment. In-center hemodialysis is usually done three times a week for about three to four hours or longer each session. In-center treatments are done at a pre-scheduled time. Some centers allow in-center self-dialysis – you dialyze at the center, but you’re able to do many or all of the procedure yourself.
You can also do hemodialysis at home where you are the one doing your treatment. People who do home hemodialysis have more flexibility about how often it can be done. If done daily, treatment time would be 1½ to 2 hours. If you and your clinician decide this is a good choice, you and a dialysis care partner will be trained how to do hemodialysis at home. Your dialysis care partner can be a family member or friend, but may also be someone you hire to assist you.
Home hemodialysis can have some advantages over in-center dialysis. It allows you to schedule your treatments to fit your routine. You can have more independence and control of your own treatments. You can also have the comfort and privacy of being in your own home during treatment. However, home hemodialysis might not be a good fit for everyone. You need to be willing to be responsible for your own treatment. As long as you and/or your care partner can pass the training and learn to place your needles, you should be able to do home hemodialysis.
Conventional versus short daily and nocturnal dialysis
Three types of home hemodialysis can be performed at home. They are:
Conventional home hemodialysis: You do this three times a week for three to four hours or longer each time.
Short daily home hemodialysis: This is usually done five to seven times a week using new machines designed for short daily home treatment. Treatments usually last about two hours each.
Nocturnal home hemodialysis: Long, slow treatments done at night while you sleep. You may do this kind of dialysis six nights a week or every other night. Treatments usually last about six to eight hours.
Whether it’s home or in-center, dialysis treatment might cause people to feel headaches, nausea, cramping and feeling “washed out” after a treatment. Generally, with doing dialysis more often, less fluid needs to be removed each time, which can help reduce some of these symptoms. Reports also indicate that people using short daily and nocturnal home hemodialysis can have fewer and shorter hospital stays, and have a better quality of life.
Whatever treatment option you choose, it is important to know if you are getting the right amount of dialysis. Tests should be done regularly to check the amount of dialysis you receive. For more information, speak with your healthcare team.
What is peritoneal dialysis?
In peritoneal dialysis, the blood is cleaned inside your body, not outside as with hemodialysis. The inside lining of your own belly acts as a natural filter. You will need a minor operation to place a catheter in your abdomen (belly) for access. During the treatment, the abdominal area (called the peritoneal cavity) is slowly filled with dialysate (dialysis fluid) through the catheter. The blood stays in the arteries and veins (blood vessels) that line the peritoneal cavity. Extra fluid and waste products are drawn out of the blood and into the dialysate.
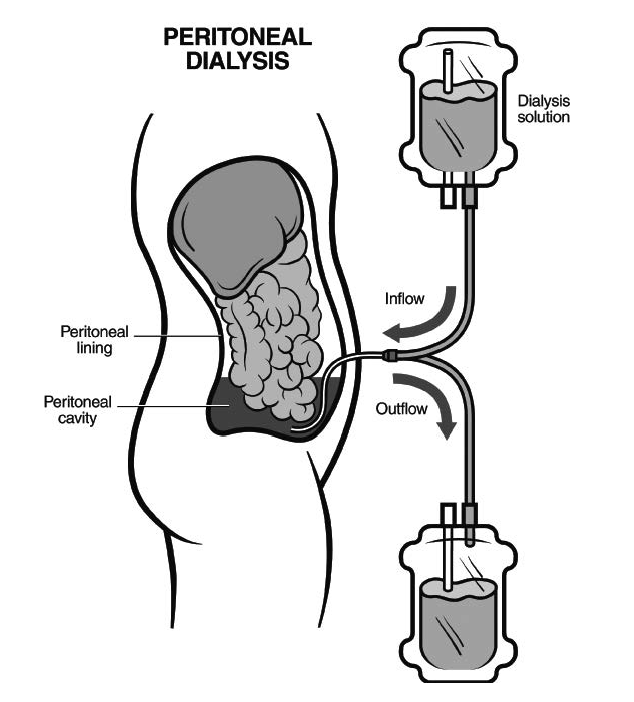
There are two kinds of peritoneal dialysis:
Continuous Ambulatory Peritoneal Dialysis (CAPD): With CAPD, you do the exchanges yourself three to four times a day. There are no machines. You put a bag of dialysate (about two quarts) into the peritoneal cavity through the catheter. The dialysate stays there for about four or five hours before it is drained back into the bag and thrown away.
Automated Peritoneal Dialysis (APD): ADP is usually done at home using a special machine called a cycler, which delivers and then drains the cleansing fluid for you. Treatments are usually done at the night while you sleep.
You can watch the following video for more information on peritoneal dialysis, including CAPD and APD.
Considering dialysis: what can I do?
If dialysis is an option, whether you choose it a long-term treatment for kidney failure or if you need dialysis while waiting for a kidney transplant, you should consider the following:
Find out as much as possible about dialysis through local support groups, written materials and educational classes
Ask your healthcare team to learn more and for help finding peer support. You cans also contact an organization such as the National Kidney Foundation
Ask your healthcare team about visiting a dialysis center
Discuss what you learn with family or close friends and share your thoughts with them
If you choose dialysis, ask your healthcare team about the following:
What types of dialysis are right for me?
If I choose hemodialysis, is a fistula the right access for me?
What about vein preservation?
Is home or in-center dialysis right for me?
If I choose home hemodialysis, is short-daily or nocturnal dialysis better for me?
Am I a candidate for incremental dialysis?
Do I have residual kidney function? If yes, how do I preserve it when I start dialysis?
You can watch this video about someone sharing share their experience about dialysis.
Content on HealthUnlocked does not replace the relationship between you and doctors or other healthcare professionals nor the advice you receive from them.
Never delay seeking advice or dialling emergency services because of something that you have read on HealthUnlocked.