ART How Should We Monitor Patients During Surveillance?
Summary; 6 years old but still representative of the low usage of multi parametric mpMRI in the detection of prostate cancer in lieu of traditional SOC methods, i.e., DRE and PSA. I was on AS (active surveillance) for 10 years before my treatment. Its frustrating for me as I had an Anterior tumor (transition zone, front lobe) that was not detected by neither of the 2 Urologists who cared for me. My primary was happy to let my PSA just keep going up; by luck my alternate URO recommended a mpMRI ‘if it made me feel better.’ I don’t know where I would be today if I had not acted on the latter’s recommendation and pushed for a mpMRI…
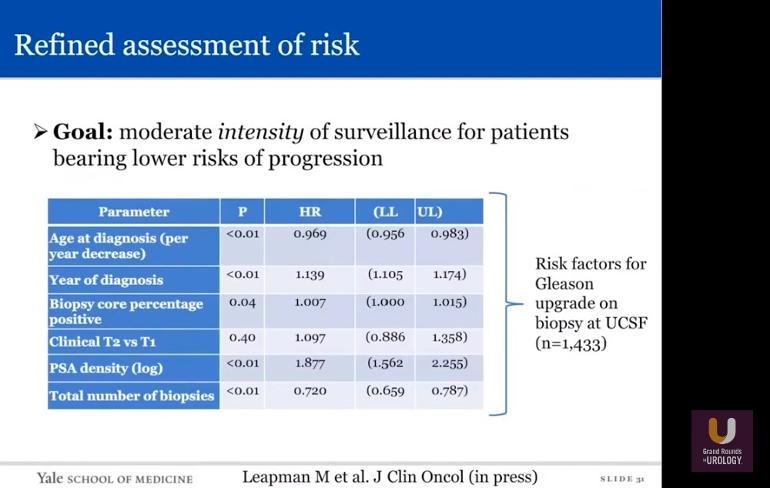
Then I also see that PSAd density is a much better predictor or PCa progression than PSA alone…was never told to develop this metric during my surveillance. Further that repeat biopsies are almost always worse; its rare that they are downgraded (MIN 4:28). There is no upside (better results) in biopsies, meaning that PCa continues to grow, morph and change for the worst over time, GS 3+3 becoming more aggressive…what else explains this. Its not an error in sampling which would be reflected in equal Upgrade vs Downgrade chances. P.S. is the chance of Upgrade via repeat biopsies ‘cumulative’ in its probability! I hope not.
But even 6 years ago the SOC called for a mpMRI if a Anterior tumor was ‘suspected.’ OK, so how do we ‘suspect’ this condition? Not by use of a mpMRI; it’s not mandated by SOC for AS in this podcast! Also, not by PSA kinetics (PSA doubling), also considered unreliable…its not clear at all in this podcast just how the heck you ‘suspect’ that a tumor is growing where a DRE cant feel it (like it did for me)…its amazing that the SOC does not just use a mpMRI as a standard detection protocol. Instead (not making this up) exploratory biopsies are suggested every 2-5 years to probe and find out if any PCa is growing (MIN 10:37)! So to understand this, if you break your arm an x Ray alone should not be used to prove you’ve got a broken bone, but every 2-5 years if symptoms persist it would be OK to cut you open to inspect the arm to make sure your pain is not from a facture…makes no sense. A lesion noted on a PIRAD 3+ mpMRI at any time is proof enough that you may have a tumor that needs a targeted biopsy! Why waste time with DRE’s and routine biopsies that don’t find all tumors and PSA totals which even at low values, like at 4.0, can mask large growths and lethal cancers (as in my case). P.S. noted again at MIN 13:36 that the consensus of using mpMRI is "changing," ya think! P.S.S. searched the Web to see what this 'change' could be, but as of yet cant find that it includes putting the mpMRI on the SOC regime for AS.
[Any notes below in square brackets are my editorial comments.] The rest of the text is my best attempt at describing what is presented. I do these summaries 1) if you don’t want to listen to the podcast and so by 2) using word searches to find terms, or words that interest you, then jump to that section.
Podcast Highlights Extracted per Minute (MIN):
MIN 1:13 AS Defined – “For men with low risk GS <6 localized PCa.” [News to me…many in this group are not in this circle of staging, yet practice AS.] 40% of all PCa cases are subject to AS in USA.
MIN 2:49 PSA Levels – PSA levels are allowed to reach 10-15 in all studies (save one) while GS is not allowed above 3+3 (except one study).
MIN 3:28 Core Results – Cores for AS patients must be low volume; <50% single core and <33% total cores positive. PSA must be “stable.” [This defines for this podcast “Low Volume” PCa.]
MIN 4:28 Biopsy Upgrade – Biopsies are upgraded (worse results) over time. The chance of Upgrade on repeat biopsies is never less than 21% and can be as high as 30%! Downgrading is rare.
MIN 6:03 PCa Specific Survival n MET vs Monitoring – No difference in 10 year PCa SS between treated (RP n RT) and monitored Pte’s (patients) but 2 fold increase risk for PCa progression n MET in monitored vs treated group over 10 years (p = 0.004). [Logical that treatment via RP and RT reduces risk for progression n MET over AS monitoring alone.]
MIN 9:20 Regimen for AS NCCN – PSA total each 6 months (PSAd not mentioned), DRE and/ or Biopsies annually, and MRI if Anterior (forward side of Prostate) tumor suspected via PSA increases n negative DRE! [This was my case; PSA kept going up and DRE’s were negative. I pulled trigger for a mpMRI at PSA 4.0 way too late. PSA kinetics (doubling) is not considered reliable, so how else would a mpMRI be called then; madness].
MIN 10:37 pMRI Assessment – Should not be used alone as an assessment tool. But, a 12 core TRUS biopsy (Bx) with anterior core samples should be considered every 2-5 years! [In the end I would have been happy to have done this! I had neither a mpMRI or exploratory Bx’s.]
MIN 12:34 PSA Kinetics – PSA doubling has not proven to correlate with progression and negative outcomes. [Other studies I have seen disagree with this finding.]
MIN 13:36 mpMRI Consensus for Use – Still not part of the AS protocol and not mandated by major guidelines of institutional protocols. [Barring positive DRE’s, Biopsies every 2-5 years are part of the SOC but a simple scan showing the cross section of the gland is not…]
MIN 13:55 Higher Risk Predictions – Main two predictors for high risk PCa are PSAd density and Negative Confirmatory Biopsy. [Your risk goes up as negative biopsies accumulate! See MIN 4:28.]
MIN 16:18 Risk Assessment Parameters- HR (hazard ratios) for AS monitoring testing shows most are around 1.0 or less except one; PSAd (density) HR 1.877, with a p=0.01! PSAd density is the amount of PSA per ng/ml you have per cm3 of prostate. [I never once got a PSAd test; never heard of one till now. P.S. a HR of 1.0 is a coin toss; 50-50 chance.]
MIN 18:44 Role of mpMRI during AS – High grade disease can be found via MRI w PIRAD >3 positive results. Study of 166 patients scanned in repeated mpMRI’s showing image progression (lesion size, diameter, shape) had positive targeted confirmatory Bx (biopsies) 44.9% of the time vs 30.9% who had a biopsy alone without a mpMRI (45% increase in finding PCa!)
MIN 24:50 Oncotype DX GPS Genomic Testing of Tumor Tissue – Changes in Oncotype DX GPS scores were compared with GS progression on repeat biopsies. GPS scores did not correlate with GS progression. [No discussion of other Genomic tests like Decipher.]
MIN 27:11 mpMRI n Genomic Testing as Predictors – Positive mpMRI loosely correlated with higher Oncotype DX genomic scores (not significant). Negative mpMRI results do not benefit from Genomic testing.