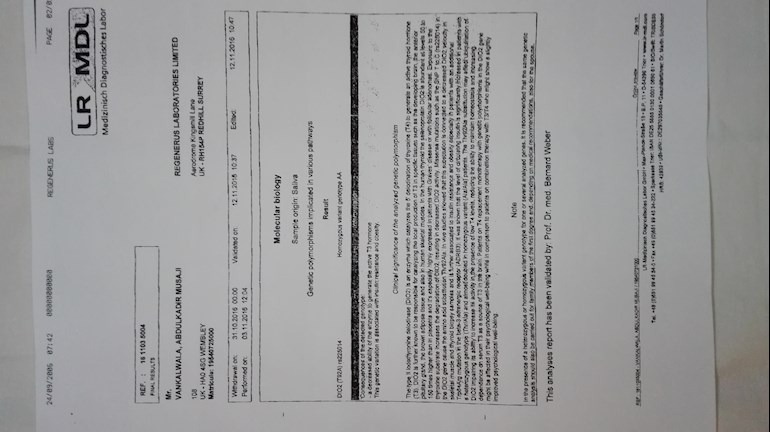
I have done DIO2 test to confirm if I have T4 to T3 conversion problem. Please see attached result and advise what next step I need to take to help with my Hypothyrodism.
DIO2 Test Result help required: I have done DIO... - Thyroid UK
DIO2 Test Result help required
HelloAPsnotFab,
Thank you for your reply. Please see following as requested.
Help with Blood test results
KadirVankalwala a month ago 7 Replies
May I request help with GENOA LAB Thyroid Function blood test results as below:
#Central Thyroid Regulation & Activity Peripheral
Total Thyroxine (T4)............. 70 (58-161 nmol/L)
Thyroid Stimulating
Hormone (TSH) 4.22 (0.40-4.00 mIU/L)
Free Thyroxine (FT4) 10.8 (11.5-22.7 pmol/L)
# Peripheral Thyroid Function
Free T3 (FT3) 5.7 (2.8-6.5 pmol/L)
FT4 : FT3 Ratio 1.9 (2.0-4.5 Ratio)
Reverse T3 (rT3) * 0.21 (0.14-0.54 nmol/L)
#Thyroid Auto Immunity
Thyroglobulin (TG) <20 (<= 40 IU/mL)
Peroxidase (TPO) 21 (<= 35 IU/mL)
-----------------------------------------------------------------------------------------------------------------
#Commentary
hypothyroidism. If such a condition exists, future repeat testing may be warranted.
Free T4 (FT4) is measured below the reference range, indicating a hypothyroid state, although multiple causes for
decreased FT4 are possible. FT4 measures the biologically active fraction of total T4, the majority of which is bound
by protein carriers in the serum and is therefore inactive.
In primary hypothyroidism, TSH values will be high, indicating a lack of responsiveness of the thyroid gland to TSH
stimulation. Generally in such cases, free T3 (FT3) and reverse T3 will also be low or low normal. The ratio of FT4 to
FT3 may be depressed since the body will preferentially make relatively more T3 in an attempt to compensate
partially for low total thyroid hormone production.
Thyroiditis can also present a laboratory picture of primary hypothyroidism. In addition to low FT4, low FT3, and
elevated TSH, anti-thyroglobulin, anti-thyroid peroxidase, or anti-TSH antibodies may be elevated, blocking the
production and release of thyroid hormone.
If TSH is also below the reference range, pituitary involvement must be suspected. In classic secondary
hypothyroidism, TSH production from the pituitary is low and thus T4 production is low. In extremely rare cases, thyrotropin-stimulating hormone production is low indicating tertiary hypothyroidism.
Prescription drugs like corticosteroids (e.g., prednisone) and dopamine can suppress TSH production, leading to
reduced T4 production. Phenytoin (dilantin) therapy can lower T4 and T3 levels, but TSH levels are usually unaffected.
Cushing's syndrome can also lead to low TSH and FT4 levels.
Free T3 (FT3) is measured to be within the reference range. FT3 measures the biologically active fraction of total T3,
the majority of which is bound by protein carriers in the serum and is therefore inactive. T3 is 3-5 times as
physiologically active as T4, and 80% of the circulating T3 is from the peripheral conversion of T4 predominately in
liver and kidney.
Reverse T3 is measured to be within the reference range.
Levels of anti-thyroglobulin antibodies are within the reference range. Thyroglobulin (Tg) is a large glycoprotein
synthesized in response to TSH stimulation. T4 and, to a limited extent, T3 are produced when tyrosine residues in Tg
are iodinated and coupled together under the action of thyroid peroxidase (TPO). Subsequent proteolysis of Tg in
cellular lysosomes allows for the release of T4 and T3 from the thyroid gland into the systemic circulation.
Levels of anti-thyroid peroxidase antibodies are within the reference range. Thyroid peroxidase is a heme-containing
enzyme that is necessary for the oxidation of iodide ions and for using hydrogen peroxide for the incorporation of these iodide ions into the tyrosine residues of thyroglobulin.
--------------------------------------------------------------------------------------------------------------------------
THESE ARE THE BLOOD TEST DONE BY MY GP - (BY NHS )
Serum total bilirubin level 7 (0.00 - 21.00umol/L)
Serum ALT level 25 (10.00 - 50.00 IU/L)
SERIUM FOLATE - NORMAL - NO ACTION
Serum Folate-(SSS) 17.7 (3.9 - 20ug/L)
Serum Ferritin-(SSS) 163 (30.00 -400.00ug/L)
FULL BLOOD COUNT - FBC - ABNORMAL - CONTACT PATIENT
Haemoglobin estimation 124 (130-170g/L)
Red Blood Cell (RBC) count 4.26 (4.40 - 5.8x10^12/L)
Haematocrit 0.4 (0.37 - 0.5L/L)
Mean Corpuscular volume(MCV) 93 (80 - 99 fL)
Mean corpusc. haemoglobin(MCH) 29.1 (26 - 33.5pg)
Mean Corpusc. Hb. conc.(MCHC) 313 (300 - 350g/L)
Red blood cell distribut width 13.8 ( 11.5 - 15 %)
Platelet count 255 (150 -400x10^9/L)
Mean platelet volume 9.7 (7 - 13 fL)
Total White Cell count 5.5 ( 3 - 10x10^9/L)
Neutrophil count 2.3 ( 2 - 7.50x10^9/L)
Lymphocyte count 2.3 (1.5 - 4x10^9/L)
Monocyte count 0.5 ( 0.2 - 1x10^9/L)
Eosinophil count 0.3 ( 0 - 0.4x10^9/L)
Basophil count 0.0 ( 0 - 0.10x10^9/L)
Percentage neutrophils 42.3 %
Percentage lymphocytes 41.8 %
Percentage monocytes 9.9 %
Percentage eosinophils 5.8 %
Percentage basophils 0.2 %
BONE PROFILE - ABNORMAL - CONTACT PATIENT
Serum alkaline phosphatase 50 ( 30 - 130 IU/L)
Serum Albumin 44 (35 - 50 g/L)
Serum calcium 2.33 (2.15 - 2.55mmol/L)
Serum adjusted calcium conc 2.37 ( 2.20 - 2.6mmol/L)
Serum inorganic phosphate 0.76 ( 0.8 - 1.5mmol/L)
SERUM VITAMIN B-12 - ABNORMAL - CONTACT PATIENT
Serum Vitamin B12 850 ( 197 - 771ng/L)
SERUM 25-HO VITAMIN D3 LEVEL - NORMAL - NO ACTION
Serum total 25-OH vit D level
interpretation 61 ( 50 - 140nmol/L)
25-Hydroxyvitamin D2 level 15 nmol/L
25-Hydroxyvitamin D3 level 46 nmol/L
HbA1C LEVEL - NORMAL - NO ACTION
HbA1c levl - IFCC standardised 38 (27 - 47mmol/molHb)
SE PROSTATE SPECIFIC Ag LEVEL - NORMAL - NO ACTION
Se Prostate specific Ag level 3.12 ( 0 - 4.1ug/L)
RENAL PROFILE - NORMAL - NO ACTION
Serum sodium 141 (133 - 146 mmol/L)
Serum potassium 3.8 (3.5 - 5.3mmol/L)
Serum urea level 3.6 (2.5 - 7.8mm0l/L)
Serum creatinine 79 (62 - 106mol/L)
GFR calculated abbreviated MDRD >90
THYROID FUNCTION TEST - NORMAL - NO ACTION
Serum TSH level 3.98 ( 0.27 - 4.20mlU/L)
SERUM LIPIDS TEST - ABNORMAL - Contact Patient
Serum triglycerides 1.3 ( 0 - 2.3mmol/L)
Serum Cholesterol 6 (2.3 - 4.9mmol/L)
Serum HDL cholesterol level 1.4 ( 0.9 - 1.5mmol/L)
Serum cholesterol/HDL ratio 4.3 ( 0 - 4 )
LIVER FUNCTION TEST - NORMAL - NO ACTION
I am feeling better compared to last year by supplementing t3 only 6.25mg dose once early morning. I tried to increase the dose but makes feel more drowsy, almost keep me a sleep all day & night. At present I can keep awake for at least 12 - 16 hours per day and do light work but my digestion of food is taking longer & longer & I am down to one light breakfast & medium meal during 24 hours. I am supplementing with HCL with pepsin & other for protien digestion for each meal.
I saw my GP last week and he says all my test are normal and nothing to worry, except he is concerned on Cholesterol level and want me start on Statin Tablets although it is coming down compared to last year & year before results. Please advise as much as you can which will really appreciated.
If the OP cannot convert T4 to T3, what is the point of taking T4? It is just going to convert to rT3, which won't help anything. NDT isn't a good idea. And, it really doesn't matter how low his FT4 is, because he's on T3 only.
K1V1 , your TSH is much too high, even on the NHS test. So you need an increase in dose.
Does the doctor know that you're on T3 only? If so, he should be testing the FT3. Once the TSH goes below one, the TSH will no-longer be of any use for dosing. It's the FT3 you should be looking at.
Your vit D3 is a bit low. You'd probably feel better if it was around 100.
As far as I understand what is written in your report, yes, you do have problems converting T4 to T3. So, the only thing you can do, is carry on with your T3 monotherapy. But, also, optimise your vit D3. 
Hello Greygoose,
Many Thanks for replying, really appreciated. I am self medicating t3 only as my GP will not provide. Also I have started supplementing D3 5000 IU & Iron (HVP Chelate 25mg). I have added 6.25 mg of t4 Levothyroxin, but I think I should increase another 6.25 mg of t3 to bring down THS to below 1.0
I will be in touch in next 4 - 6 week time to see how these changes improves my health.
Many Thanks,really appreciated.