It makes a little more sense now.
A bit of a explanation on my being stage 4 ... - PBC Foundation
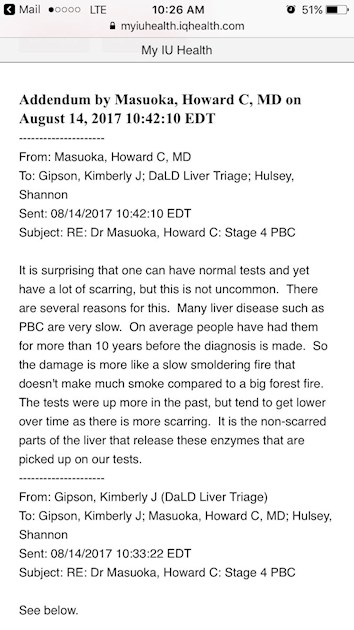
A bit of a explanation on my being stage 4 but having a, almost normal, hepatic panel
Hi
I don't quite understand this!
I am stage 3 but my ALT has been in 1000s!
Can you help me understand. 😘
Mine is still high, but as close to normal as it has been in quite some time. When I was diagnosed mine was in the 2000's. That was in 2012. Go back through my posts & look at the numbers I've posted from my most recent hepatic panel. I started taking Ocaliva 5mg in June. I take it with the Urso 1000mg daily. My heptologist has me on a standing lab order for every two weeks for six weeks, then monthly. Basically to make sure the Ocaliva is helping. He is also gradually increasing my Ocaliva to 10mg. This has been a godsend so far. My numbers have never looked so good.
Thanks for sharing this as I have felt so ill so many times and the doctors response is always that my labs are normal now it all makes sense can I copy this to give to my doctor?
Thanks ahead!
Hi,
but....hmmm..this cannot mean that if the Tests show big values ("...tests were up more in the past but tend to get lower over time as there is more scarring....."), your Liver is good condition(still)????
Higher the Enzymes (ALP, Blirubin...AST, ALT, etc...) better the Liver????
Or with some other words:
Higher the values: There is a big fire in the forest.
Lower Values: Few trees left (still burning)
That simple?
I'm a bit sceptical
Betonarme I thought the idea was to have low ALT, ALP etc?
It can be possible. Since the dead part of liver doesn't make anything.. well, low numbers are low and it is good !
Cheer up!
This may not be exactly what you are discussing here, but as with most things to do with PBC, nothing correlates with anything, particularly the enzyme levels with the progression of damage to the liver. While the doctor's response below is 'dated' it holds true for my experience - I'm Stage 4 with advanced cirrhosis and now have the best LFTs I've ever had since diagnosis 28+ years ago.
"Howard Worman, MD
Division of Digestive and Liver Diseases
Departments of Medicine and of Anatomy and Cell Biology
College of Physicians & Surgeons
Columbia University
New York, NY 10032
December 1999
Question
Is it possible to be in stage 3 or 4 by the biopsy and have normal LFTs taking Actigall or URSO? Are the LFTs actual indicators of the disease progress?
Answer
I always tell the second year medical students that "liver enzymes are NOT liver function tests (LFTs)." The term "LFTs" is a terrible one and really should not be used. [Help me convince your doctors!]
The values of the blood ALT, AST, alkaline phosphatase and gamma-glutamyltranspeptidase (GGT) activities do NOT tell you about the function of the liver. They also do not tell you about disease progression (i.e. the development of cirrhosis or deteriorating liver function). The so-called "LFTs" can be normal in individuals with end-stage liver disease.
In contrast, they can be markedly elevated in individuals with liver disease but normally functioning liver. In PBC, ursodiol (Actigall or URSO) may lower the blood alkaline phosphatase activity in the setting of significant liver damage (Stage III or Stage IV histology).
The best biochemical tests of liver "function" are serum albumin concentration, serum bilirubin concentration and prothrombin time. In PBC, the serum bilirubin concentration (which may also be lowered by ursodiol) is probably the best biochemical predictor of disease progression."
This was taken from the Pbcers.org "Doctors Panel Answers PBCers Questions" web site some years ago (by me) but I can not provide the link as the site is being "updated".
My hepatologist said the liver enzyme tests actually do give them a very good idea how the liver is functioning.
I'm not trying to argue with anyone here but I have been worried about this very issue. So asked him about that.
Pam
Hi,
I really appreciated your second to last paragraph explaining the best biochemical tests of liver function. It has given me a base line of how to ask my doctor how to determine how I am progressing. He doesn't share much and states "what difference does it make if we are not going to change your treatment plan". I am sure he has my best interest best interest at heart and wants to keep me as positive as I can be. But I would really like to know because my plans would change a lot if I thought I only had a year or two before I couldn't do those thing. and if I think I have 10 to 15 years I would conserve the little dollars I have and not take those trips to visit family.
If you don't mind my asking...... what does stage four feel like and is your doctor able to give you some idea how much time you have before needing a transplant? What has your doctor said about acute symptoms to look for that means it is time to go to the Emergency Room as a result of entering liver failure.
I know this is personal. I appreciate anything you feel you can share. You are a veteran pro and a wealth of information that us newbies really appreciated what ever you might wish to share.
Warm Hugs,
Kathy
Hi Q8Cooper,
First off, there is no standard time frame with PBC - my cousin and I were diagnosed the same year (our biopsies indicated we were both Stage 2), while she had a transplant two years ago I'm still plodding along. My doctor has not talked to me about a transplant because I am no longer eligible for one - I'm in Australia and our cut off age for liver transplants is 70, I turned 71 last July.
"How does stage 4 feel" hmmm..... I'm guessing you want to know are there any warning signs/symptoms that alert you to the beginning of the cirrhosis stage - for me there were no obvious changes. My first indication was when I couldn't play hop-scotch with my grandchildren, and bouts of nausea. After discussing this with my specialist I was sent for an ultrasound which indicated cirrhosis (bit of a shock for me), and then I had a fibroscan which gave a result of 30 )(shock for me and my specialist) - I now have many of the complications associated with liver cirrhosis.
Just remember we all progress, and experience PBC differently so your journey will not necessarily follow mine, or any other person's for that matter.
I don't mind telling my story (that's pretty much how we all learn about this condition), so if you have any other question ask away. 😃
I agree with DianneS,
if you do a google search for "MELD Score" you will see why. MELD(Model for End Stage Liver Disease) is calculated as:
MELD = 3.78×ln[serum bilirubin (mg/dL)] + 11.2×ln[INR] + 9.57×ln[serum creatinine (mg/dL)] + 6.43
So what we have here is Bilirubin and INR and ceratinine. These are all a measure of how good liver is working, INR is "international normalized ratio for prothrombin time".
I think this has something to do with blood clotting.
Higher MELD values are not a good sign. So, there is no ALP, AST, ALT here.
ALP, AST, ALT are something to do with ongoing current liver damage. It says something bad is happening in the liver, but liver can be very well working, I would say even regardless of the Disease stage. I think ALP, AST, ALT etc. goes also higjh when people get a acute liver damage due to toxins, alcohol, Virus infection etc.
I am not sure if all I wrote is correkt but I have the feeling it should be like this more or less.
We already know pbc is a progressive disease which doesn't have cure tho it can be contained with proper medicine!
alt,ast and alp won't tell you liver cirrhosis stage but they will definitely tells you how your liver is functioning !
Yes, Albumin and bili can be proper marker for damage liver along with alt ast and alp that's why hepatic panel have these test total protein, albumin, tbili, Dbili, alt, ast, alp..
Brief description of what these test mean
Albumin measures the protein from liver
Bilirubin produce when liver breaks down red blood cell
Total protein are combination of albumin and globulin
Alt and ast are enzymes produce my liver
Alp is produce by liver, body tissue and bone
So alt, ast and alp give you like a warning if something bad happen to liver..
This is how I understand about hepatic panel
Here is a link to the Mayo Clinic's information on LFTs - this may help people to understand what the Liver Function Tests are all about. 😊
mayoclinic.org/tests-proced...
Mayo and mine statement match if you notice 🤗
Yes, I did. 😀
Dianne,
how long pbc people can live normal life after diagnosed, do you have any idea or story to share?
Sachin 1234,
"how long pbc people can live normal life after diagnosed" - difficult question to answer as we are all different, and/or diagnosed at different stages of PBC.
I can't speak for others, but I can contrast my cousin's and my journey with PBC. But first I think I should clarify something, though my cousin and I are both Americans, I have lived in Australia since the age of 10, so our medical treatment was slightly different. As I mentioned above, my cousin and I were diagnosed the same year (28 years ago), our respective biopsies indicated that we were both in Stage 2. At the time of diagnosis I only suffered fatigue whereas my cousin had already developed 'Gastric Antral Vascular Ectasia (Watermelon Stomach)', so she did not actually have a 'normal' life after diagnosis. I on the other hand, cruised along with the fatigue and the odd bouts of 'itch' for 20 years - I really didn't give PBC much of a thought during that time. Thinking about it now, even though the fatigue was a constant it didn't really impact my life that much - I think you'll find that most of us who suffer the fatigue unconsciously learn to pace ourselves. Approximately 8 years ago my 'normal' life began to crumble, as I said in an earlier post, I first realised things had changed when I couldn't play hop-scotch with my grandchildren, my muscles had weakened - I have since developed a number of the complications of liver cirrhosis. Now I only have about 5 hours a day that I can get things done, the rest of the time I'm laid out like a 'beached whale'. 
I'm sure there are others here who can add their stories, and each one would be similar, yet different. The complexities of both the individual, and PBC, makes it almost impossible to give any standard time frame for the stages, or normal life spans.
Take care.
Di
Thank you for your answer..
I know, it is going to be tough that's why right now, I'm living the life..my dr motivates me to live normal life as well but once in a while I get nightmares and that makes me down. I'm 40 now and I hope I will make it 60 without any problem after that I don't care🙏🙏🙏❤️❤️🤗🤗
I wouldn't normally do this, but here is the excerpt on liver biochemistry from the PBC Foundation's compendium, "Living with PBC". It is available free online to all members of the PBC Foundation.
Liver Biochemistry
When we think about liver biochemistry and PBC, there are a number of points that need to be kept in mind.
• Liver biochemistry doesn’t necessarily give a good idea of liver function
• Many of the tests important to PBC are not exclusive to PBC
• There are many reasons for changes in liver biochemistry that have nothing to do with PBC
• Trends give more information than just one set of biochemistry results
• Different labs will have different standards for “normal”
• The normal range for many of these tests will also vary with age, ethnicity, and gender
So, to obtain a good idea of how the liver is working, we need to look at a number of test results and compare them to previous results. Ideally, each patient would keep an eye on their blood test results so they know if, and how, their PBC is progressing. Please note that some “normal” ranges are in brackets. These are just a guide and only incorporate the most commonly used measurement units (such as iu/L).
ALP (iu/L: 40-130 adult males and 35-105 females)
ALP is short for Alkaline Phosphatase or Alk Phos. ALP is an enzyme made in the liver and also in bones, placenta, kidney, and intestine. It can be raised in liver disease, e.g. in cholestasis, but also in some bone diseases and other conditions. Most people with PBC have elevated ALP. For all ALP can be raised in other conditions, it is helpful in diagnosing PBC.
ALP and, in particular, its response to Urso, can tell us a lot of important information about a patient’s individual risk of disease progression. It is incorporated into both the UK-PBC risk score and the Global PBC risk score.
Bilirubin (UK: micromol/L 1-22, USA: <1.2mg/dL)
Bilirubin is bile pigment in the blood, the level of which can increase when there is too much being produced (such as in some forms of anemia), when there is damage to liver cells (hepatocytes) or when bilirubin cannot be excreted into bile (e.g. when there is bile duct obstruction). In PBC, levels of bilirubin increase as liver damage increases. Jaundice (yellowing of the skin and in the eyes) can be seen when bilirubin exceeds 40µmol/L
Bilirubin level is the best short-term marker for risk in PBC. As soon as bilirubin extends beyond the Upper Limit of Normal (ULN), we would hope each patient is referred on to a specialist liver unit for specialist screening and monitoring.
Albumin (g/L 35-50)
Albumin levels can, in part, give us an idea of how well the liver is working. Albumin is a protein which is made by hepatocytes but may be lost through the kidneys, skin or the bowel. When there is illness, or infection, in the liver the production of albumin may fall. So, the level of serum albumin does provide a measure of how well the hepatocytes are working, but does not tell us the degree of cell damage to the bile ducts.
ALT (iu/L 5-31) and AST (iu/L 4-43)
Alanine aminotransferase (ALT) and Aspartate aminotransferase (AST) are enzymes found inside hepatocytes. They can be slightly raised when there is inflammation in the liver (commonly found in early PBC). As damage to hepatocytes increases in severity and rate then these levels will increase more so. Both these enzymes are found in many other cells and so high levels can occur in many forms of tissue injury.
Sometimes the ratio between ALT and AST can give the clinician helpful information, as can a sudden drop from elevated levels. Similarly, very high levels of ALT/AST may direct the clinician to alternative conditions which would need to be diagnosed.
GGT {γGT} (iu/L 7-40 female and 9-50 male)
Gamma (Greek letter γ) glutamyl transferase is an enzyme found within the cells of the liver. Commonly raised in PBC, it is a non-specific test and can be found to be raised in many conditions that affect the liver. Raised GGT is often associated with excess alcohol intake, which will often lead to the uncomfortable question of how much does a patient drink.
Prothrombin
Prothrombin is a measure, in a laboratory, of how long blood takes to clot under specialised conditions. The clotting time recorded is a reflection of many different clotting factors. Nearly all clotting factors are made in the liver. A prolonged clotting time may be a consequence of liver damage but it may also be a reflection of low vitamin K levels.
Vitamin K is a fat soluble vitamin which is absorbed from the bowel. Some people with PBC, who do not absorb fat well, may find their vitamin K may go straight down the loo rather than reach their blood. Prescribing vitamin K may improve clotting time.
Overall, liver biochemistry is just one part of the assessment of the person with PBC. Whilst there is much information to be gleaned from a series of tests over time, it must be remembered that a PBC patient is a person whose life needs to be looked at as a whole in order to find the best answers for that individual, their family and their PBC. As ever, if you have any concerns about your blood tests, please ask them to explain the tests in more detail.
I hope that helps.
Robert.
Thanks Robert, that pretty much matches the Mayo Clinic's information I posted above.
I have the 'compendium', received it a few years ago when I first joined the Foundation - I must open the file and reread it. Oh, by the way, has the compendium been 'updated' lately, or is it likely to be? There has been quiet a bit of research happening since I first received my copy.
Don't go back and read the old one!!
The excerpt is from the new compendium. It is available on the Foundation website and will be an integral part of our brand new app about to be released for PBC Day (10th Sept).
Thanks, I'll delete the 'old' and download the new. As far as the app is concerned, will it be available for an 'android' tablet? I don't have, nor use, mobile phones - old fashioned I know, but when I'm out I don't want to be taking phone calls. 
let me find out... the app will operate on ios first. I *think* this means apple devices of any kind but I need to check that. Mid-Sept, I have been promised the android version. I shall check if that is phone only.
I am not quite so old fashioned but pretty close: hanging on to my trusty blackberry!!
Our understanding is that both the ios and android versions will adapt to other devices using the same system. So, I am hoping that means you can use it on your android tablets, PCs, etc...
Am I alone in finding that a little discouraging? How else do we monitor how we are doing if the blood tests aren't really giving us the real picture?
This is why we ask our experts these questions. I also recently found out my stage of cirrhosis is at F2, & activity of inflammation is at A2. Just the beginnings. That's how I understood it anyway🤓