Often overlooked and misdiagnosed, silent reflux affects over 50 million Americans. The backflow of stomach acid and digestive enzymes (pepsin) can wreak havoc on your esophagus (the food passage that goes from your throat to your stomach), as well as your ears, nose, throat, vocal cords, sinuses, mouth, and lungs. Pepsin, in the presence of acid, digests protein and damages tissue. Outside the protected stomach, pepsin, bathed in acid, digests you! And when pepsin attacks your sensitive airway and esophageal tissues, you can suffer all kinds of problems.
The most common silent reflux symptoms are hoarseness, chronic cough, throat-clearing, post-nasal drip, sinusitis, sore or burning throat, difficulty swallowing, shortness of breath, snoring, sleep apnea, bad breath, tooth decay, asthma, and COPD. Unfortunately, your doctor is probably unaware that these symptoms may be caused by silent reflux and that it could be controlled with the proper diagnosis and treatment.
Did you know that asthma is one of the most common misdiagnoses, because silent reflux mimics asthma? Here’s a big tipoff: When you have trouble breathing, do you have more difficulty getting air IN or OUT? People with reflux have trouble getting air IN during inspiration (not out during expiration). People with asthma have difficulty getting air OUT of the lungs. In truth, many people with “asthma” may not actually have it, and, consequently, asthma medication doesn’t really help much if at all. The fact is that once the correct diagnosis is made, effective anti-reflux treatment can permanently cure this asthma-like breathing problem.
How Do I Know If I Have Silent Reflux?
One of the characteristics of silent reflux is that most people who have it have several different symptoms all at the same time, but often heartburn isn’t one of them.
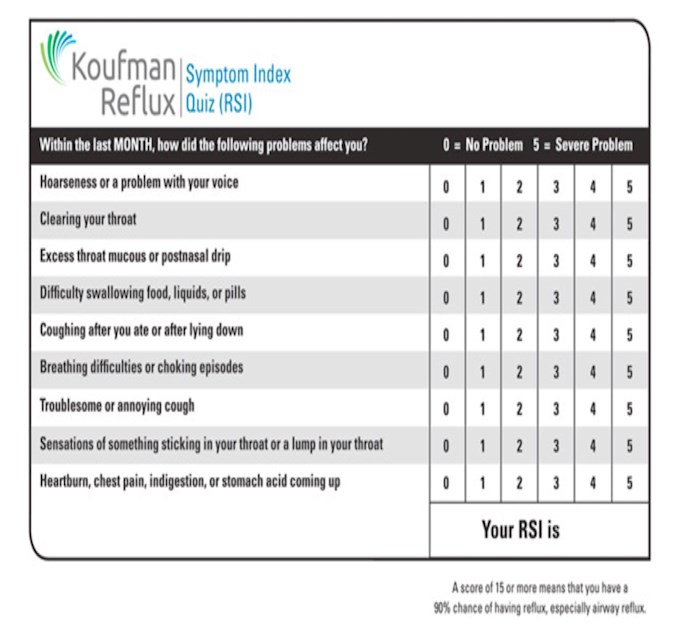
To find out if you may have silent reflux, take this simple quiz. Just circle the number for each symptom and add up the numbers. The quiz is actually known as the Reflux Symptom Index (RSI), and it is a great first test to see if you have reflux. If your RSI is 15 or more (and you have a zero or one for heartburn), you may have silent reflux; you should see a specialist trained in detecting reflux by examination of both the throat and esophagus. Doctors who only scope the esophagus are missing the boat. Get your printable version of the Reflux Symptom Index.
Why Is Reflux Sometimes Silent?
What makes silent reflux different than heartburn is that the silent reflux sufferer may be unaware of having it, and his or her doctor may not suspect the diagnosis. A lot of reflux is needed to damage the esophagus, but very little reflux can severely damage the more sensitive throat, sinuses and lungs. Many people with silent reflux have never even once experienced classic heartburn.
How the term “silent reflux” came to be is instructive. In 1987, Walter Bo, a medical school colleague, was my patient. As a result of nighttime reflux, he had terrible morning hoarseness. This was because he had a habit of eating dinner very late and then falling asleep on the sofa. Hence, he would reflux into his throat all night.
I tried explaining the problem, but Walter repeatedly denied having reflux. As it turned out, Walter affirmed that he thought that heartburn and reflux were the same. When I was able to explain that one could have reflux without heartburn – as in this example, when it occurred during sleep – Walter rolled his eyes and said, “I see. I have the silent kind of reflux.” I declared, “Yes, Walter, that’s it! You have silent reflux!”
Why Doesn’t My Doctor Know About This?
Unfortunately, people with silent reflux symptoms, even if they ask their doctor, are usually incorrectly told they do not have reflux. The medical specialties are broken down by parts of the body, and doctors are experts in, and only test for, those parts of the body in which they specialize. The problem is that reflux does not care where your doctor trained and how it might affect the different medical specialties – the esophagus treated by gastroenterologists, the throat and sinuses treated by ear, nose and throat specialists (otolaryngologists), and the trachea and lungs treated by lung specialists (pulmonologists).
The Solution: Integrated Aerodigestive Medicine
Only a trained reflux specialist who knows what to look for in all affected areas and who has the right diagnostic tests is equipped to make an accurate diagnosis. Otherwise, a doctor may guess wrong and treat you for an illness that you don’t have. Some of the symptoms of silent reflux can sometimes be caused by other diseases, which doctors try to treat unsuccessfully, leaving you miserable, frustrated, and having wasted money on useless tests and drugs.
Instead of focusing on the patient’s diet and lifestyle – the root cause of almost all reflux disease – doctors often employ pills, usually the wrong pills, that rarely correct the problem. In truth, reflux medications are grossly misused and over-used today.