There seems to be a lot of confusion of what peak flow is, how it works and what is a ‘good’ score so I thought I’d make a post on it!
WHAT IS PEAK FLOW?
Firstly peak flow (PF) can also be called peak expiratory flow (PEF) or peak expiratory flow rate (PEFR) so any and all of these abbreviations means the same thing so don’t get confused if people write them differently!
PF is your maximum speed of expiration, so it literally just measures your ability to breathe out. It measures the airflow through the bronchi (large airways) and thus the degree of obstruction in those airways. However it won’t necessarily show restrictions in the smaller airways, and this is why some people have ‘unreliable’ PFs, as their asthma level and PF do not correlate due to their asthma not affecting the larger airways. That being said those whose asthma mainly affects smaller airways will normal have a drop of some description as there is less air in their lungs to breathe out, it just doesn’t meet with the ‘expected’ drop for the severity of attack.
When you use a peak flow meter (PFM) it measures litres per minute, but on spirometry it’s measured per second so anyone with confusion there, times it by 60 and you’ll be able to compare to your usual measurements 😉. There are many different ‘brands’ of manual PFM, as well as child ones (is a lower range). So long as it works and you’re not beating it (ie you have the kids one and your best is out of range 😉) then any is fine! I think mini-wright is the go to for most of the NHS but it really doesn’t matter! There are digital PFMs available, however there is no clear verdict on how good/accurate these are, and I think people often find they score a higher best on digital compared to manual. For this reason, whichever device you decide to use ou should stick to!
HOW TO DO PF CORRECTLY
Something that’s not always taught, but always commented on! To do it correctly you should do it standing (unless advised against this for other medical reasons), keeping the PFM horizontal (no angling up or down!), with the numbers facing up. Hold at the bottom (making sure to not impinge the moving arrows pathway!) and not the top/end. Take a big deep breath in, create a good seal with your lips on the mouth piece and blow AS HARD AS POSSIBLE! 😉😂 repeat it 3 times (with recovery if you need it) and the BEST score is the one that you count (I knew someone who thought it was the average and would then do more maths! 😅😂).
HOW DOES IT SHOW ASTHMA?
Asthma is something that’s really hard to diagnose, but one this that is known is the reversibility. For asthma (even those with unreliable PFs) if you are having issues, taking 2 puffs of salbutamol should improve your score. This is known as the reversibility test, and is sometimes carried out in GP practices, as well as hospitals etc (officially its done with spirometry and other tests, but can be done unofficially with PFMs at home). Simply put, you do PF whilst mild-moderately symptomatic, you take inhaler, you wait 15 mins (time it takes for salb to kick in), you redo PF. If you have a big enough improvement it is indicative that asthma may be the issue, if there is little/no improvement it is more likely to be something else.
WHAT IS A GOOD PEAK FLOW?
Best peak flows are personal, and should be used over and above your predicted if you know it. If you don’t know your best you should use your predicted until you’ve worked it out! The current predicted chart I think was produced in the 70s/80s from a town in Scandinavia, so may not even truly represent the average for today anyway. And it is just that... an average! Some people will be way above predicted, others will be way below! There are so many things that can affect your best score, as it will be affected by how large your lungs are. As a random example if your lungs can at max hold 1L of air you will never ever be able to blow out more than 1L, even if your predicted is 1.5L, but if you can hold 3L of air then you should be able to blow out more than 1.5L. Some of the things that can affect your best scores are; gender, height, age, weight, PF technique, standing v sitting, time of day, high level/endurance/frequent sports, playing wind instruments, singing frequently/professionally/in a choir and smoking to name but a few. Factors like sports, music and smoking have a greater effect as a child, so the changes may last into adulthood, however it will affect as an adult too. This is why it’s pointless comparing best PFs as so many factors go into it, and it truly doesn’t represent anything but how big your lung fields are. My friend and I are predicted the same PF, she has no respiratory (or any health) issues and she gets 68% predicted, I have severe asthma and I get 143% predicted! Best scores can also increase and decrease over time (age being a factor 😉), so I think they say your best only counts if you’ve hit it in the last 6 months (I get confused between 6 or 12 but think it’s 6 😅), and you should hit it multiple times to confirm its your best (can be done all on the same day 😉). Those new to asthma often find as they gain control (and practice PF technique) their best also increases... personally I think it took a year before I found my best, and had to change my plan about 6 times 😅. And yes to anyone questioning, when you get a new best, you should then adapt the numbers of when you should seek help!
WHEN SHOULD I SEEK HELP?
Everyone should have an asthma action plan (AAP) which should be filled out for you by your GP or asthma nurse. If you don’t have one you can find them here; asthma.org.uk/advice/manage.... Typically asthma plans have ‘zones’; green, yellow/amber and red. They are decided by asthma symptoms +/- PF score (if you have an unreliable PF you go on just symptoms). I am not going to go into symptoms of each zone (as they are written on the plan 😉) but will do peak flow. There is often a slight variety in % as normally the doc writing the plan is doing it individually but typically;
GREEN zone is anything above 70-80% of your BEST score (I use 75 😉)
RED zone is anything below 50-60% of your BEST score (typically it’s 50% but some brittle asthmatics have to use 60%, so don’t worry if that’s what you’re told to do). If you hit red zone you should follow the guide of what to do, and be considering going to hospital, if you manage to resolve it at home with 10 salbutamol puffs as suggested you should follow up with your GP that day or the next. If it’s the weekend, it’s worth contacting 111 for OOHs just to be checked over.
YELLOW/AMBER zone is the area between the two! This is typically when you should contact your GP, and possibly start your emergency pack of steroids if you have them. If you find you are constantly in yellow, and only return to green after reliever medication (MART or salbutamol) and it’s an ongoing issue it may be that you need to change your preventer inhaler or escalate your maintenance treatment with add ins like montelukast.
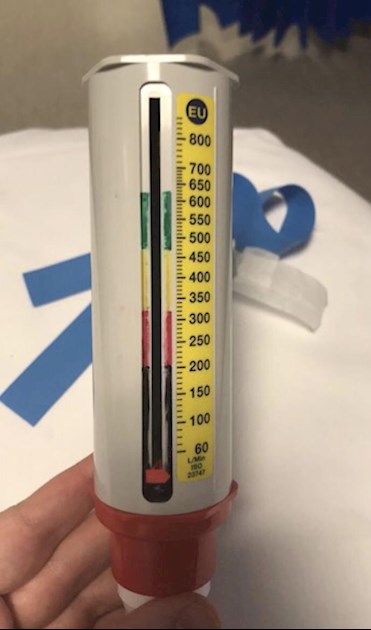
I also add in BLACK zone which is anything below 33% as that is classed as life threatening so my rules say I HAVE to go to hospital if I hit that, even if I recover with home meds (just wanted to explain why my PFM is green, yellow, red and black).
As you can see above I have added a photo of my PFM, and it usually goes down a storm with any medic who hasn’t seen it 😉. I don’t know about you, but when my asthma’s bad, I REALLY can’t do maths so this was my solution 😅😂😂. It’s easy to do and doesn’t affect the function of the PFM, just get 3 (or 4) sharpie/marker pens and colour in your zones! In times of trouble (or when in hosp with medics who don’t know your best score) it’s easy for everyone - blow and check the colour!!!
But for summary, IT’S THE % THAT MATTERS NOT THE ACTUAL NUMBER! 😅😂
SHOULD I TRACK IT?
Simply put, yes. Yes you should 😅. It is usually advised that you track your score morning and evening, and record them either in an app or on a paper diary as it’s a good way to measure your control over time and see fluctuations and trends over time, and can often help identify a problem before you are even aware of it! When you do it, you should always try to do it at the same time of day and either always before or always after your maintenance medications. You can do it both pre and post if you really want to! If you are new to asthma, or in hospital due to attack, they may ask you to track it during the day, as that helps to see if you are well controlled or not, and can also help diagnose asthma.
WHEN SHOULD I REPLACE MY PFM?
I’m talking manual here so the ones you get from the good old NHS 😉. I’m pretty sure they don’t come with any best before date (if they do then comment cause I’d have learn something new! UPDATE Singinglouder says life expectancy is about 3 years 😉), however they do wear out and get old. The internal mechanism can start to break down, which can start putting out weird and random results 😅😂. For me, I know it’s time to replace when, what I think is rubber inside starts to stick, creating a slight popping sound and normally a stupidly good PF (I once ‘beat’ a PFM of 800 due to this happening, when on a different device I was scoring under 300 😅). As soon as it’s happened once, I get organised to get another, and don’t forget you can get them on prescription if you need to!
Here’s a link to the AUK peak flow page asthma.org.uk/advice/manage... which also links further to AAP and PF diaries if you are interested.
And for those who would like to see the most commonly used predicted score chart; peakflow.com/pefr_normal_va... (I REALLY hate they call these ‘normal’ and not predicted scores 🙄😒)
Alternatively If you’re concerned or need advice about anything The AUK helpline nurses are great and can be reached on 0300 2225800 M-F 9-5. Alternatively their WhatsApp service is 07378 606728.
Hope this helps anyone with questions, and if I’ve missed anything please ask and I’ll do my best to answer/add it to the post!